Cancer Cell:研究人员成功消灭肿瘤干细胞
2013-03-25 蓝建中 新华社
日本一个研究小组发现,对肿瘤干细胞进行基因操作可以使化疗药物更易发挥作用,杀死癌细胞。这一发现或促进开发出根治癌症的治疗方法。 肿瘤干细胞被认为在体内处于几乎不增殖的“休眠状态”。化疗药物虽能遏制肿瘤细胞增殖,但对干细胞却难以发挥作用。即使化疗后肿瘤看起来已经消失,但只要残留少量干细胞,就会导致癌症复发和转移。 日本九州大学教授中山敬一率领的研究小组发现,肿瘤干细胞中一种名为“Fbxw7”蛋白
日本一个研究小组发现,对肿瘤干细胞进行基因操作可以使化疗药物更易发挥作用,杀死癌细胞。这一发现或促进开发出根治癌症的治疗方法。
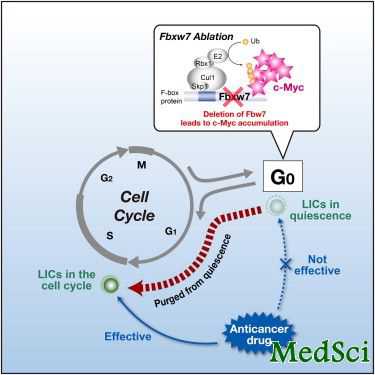
肿瘤干细胞被认为在体内处于几乎不增殖的“休眠状态”。化疗药物虽能遏制肿瘤细胞增殖,但对干细胞却难以发挥作用。即使化疗后肿瘤看起来已经消失,但只要残留少量干细胞,就会导致癌症复发和转移。
日本九州大学教授中山敬一率领的研究小组发现,肿瘤干细胞中一种名为“Fbxw7”蛋白质能够遏制细胞分裂。他们对患有慢性骨髓性白血病的实验鼠进行基因操作,使肿瘤干细胞无法再制造这种蛋白质。此后,研究人员让实验鼠服用化疗药物“格列卫”,35天后不再给药。
研究发现,一般情况下,患白血病的实验鼠60天后会有90%的复发率,而不能制造“Fbxw7”蛋白质的实验鼠复发率只有20%左右。研究小组判断肿瘤干细胞已经死亡。
中山敬一说:“如果开发出阻碍这种蛋白质发生作用的药物,同时与化疗药物并用,就有望根治癌症。”相关研究成果刊登在美国《癌细胞》(Cancer Cell )杂志网络版上。
与肿瘤干细胞相关的拓展阅读:

doi:10.1016/j.ccr.2013.01.026
Ablation of Fbxw7 Eliminates Leukemia-Initiating Cells by Preventing Quiescence
Shoichiro Takeishi, Akinobu Matsumoto, Ichiro Onoyama, Kazuhito Naka, Atsushi Hirao, Keiichi I. Nakayama.
Imatinib eradicates dividing progenitor cells of chronic myeloid leukemia (CML) but does not effectively target nondividing leukemia-initiating cells (LICs); thus, the disease often relapse after its discontinuation. We now show that Fbxw7 plays a pivotal role in maintenance of quiescence in LICs of CML by reducing the level of c-Myc. Abrogation of quiescence in LICs by Fbxw7 ablation increased their sensitivity to imatinib, and the combination of Fbxw7 ablation with imatinib treatment resulted in a greater depletion of LICs than of normal hematopoietic stem cells in mice. Purging of LICs by targeting Fbxw7 to interrupt their quiescence and subsequent treatment with imatinib may thus provide the basis for a promising therapeutic approach to CML.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#cancer cell#
34
#Cell#
28
#CEL#
39
#研究人员#
42