Cell:一种新的糖尿病相关激素被发现,有望成为新靶点
2016-04-17 MedSci MedSci原创
研究人员一开始只是想为罹患新生儿型类早衰症(NPS)的患儿寻求答案,这种罕见遗传病会阻止机体累积脂肪,结果现在却获得了一个有可能影响数百万2型糖尿病患者生活的研究发现。他们将研究结果发布在今天的《细胞》(Cell)杂志上。 论文的资深作者、贝勒医学院医学遗传学家Atul Chopra博士,首先在2013年发现了两名罹患这种罕见疾病的患者(全世界只有少数患者被描述患有此病,且病因未知)。在
研究人员一开始只是想为罹患新生儿型类早衰症(NPS)的患儿寻求答案,这种罕见遗传病会阻止机体累积脂肪,结果现在却获得了一个有可能影响数百万2型糖尿病患者生活的研究发现。他们将研究结果发布在今天的《细胞》(Cell)杂志上。
论文的资深作者、贝勒医学院医学遗传学家Atul Chopra博士,首先在2013年发现了两名罹患这种罕见疾病的患者(全世界只有少数患者被描述患有此病,且病因未知)。在那时,全基因组/外显子组测序还才刚开始被用来寻找从前无法解决的医学/遗传学谜题的答案。
Chopra长期以来对了解能量代谢疾病感兴趣,NPS患者极低水平的身体脂肪激发了他的想象力。两位患者要带着这种“神秘”的疾病度过他们的一生,当Chopra认识到测序技术可以用来攻克这一问题时,邀请了两位患者来到德克萨斯儿童医院的遗传学诊所进行了最初的访谈和测试。
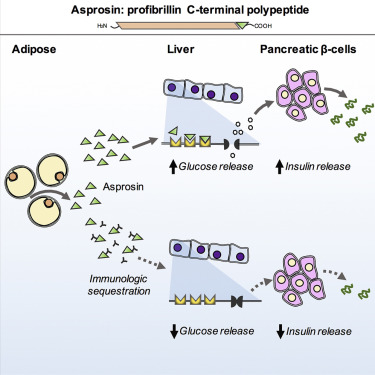
利用全外显子组测序,Chopra和同事们发现一种遗传突变似乎对NPS负责。但对于这一突变导致NPS的机制却仍不清楚。将这一问题带到实验室,研究人员阐明了这些突变阻止了患者生成一种从前未知的激素。这种新发现的激素叫做asprosin,似乎是由白色脂肪所生成,是profibrillin的C末端剪切体,在体内是纳摩尔水平。但是,当它进入肝脏后,激活 G protein-cAMP-PKA通路,使肝脏释放葡萄糖进入血流中。如果asprosin 异常低水平的NPS患者,则无法完成这一任务,显示出低血糖。
与之相反,高血糖和胰岛素的肥胖/糖尿病患者显示asprosin水平高于正常。利用这一信息,研究人员确定他们可以开发出一种抗体来对抗它,利用这种抗体来中和asprosin,这一过程就叫做免疫隔离(immunologic sequestration)。他们有可能通过这种方式来减少肝脏释放的葡萄糖量,使得胰腺细胞释放较少的胰岛素。
“我们开始想知道,这可以成为一种治疗糖尿病的方法吗?”Chopra说。
为了验证这一概念,他们用这种抗体治疗了糖尿病,发现即便单次剂量的抗体也能很好地起作用,将它们的胰岛素水平降低至正常范围。当在更长的时间内治疗这些小鼠时,它们的胰岛素抵抗完全正常化。
Chopra 说:“这一结果让我们绕了个大圈。我们从一种极为罕见的遗传病开始,利用了从这些患者处得到的信息,发现可以靶向一种新激素来治疗影响更多人的一种不同的疾病。如果人类糖尿病患者能够以与糖尿病小鼠一样的方式响应asprosin抗体,这一发现可以促成一种糖尿病新疗法。这就是研究罕见人类遗传病的价值所在。有时候,除了一开始研究的小群患者,这样的努力还可以影响更多的人。”
作为这个故事开始的其中一名NPS患者Abigail Solomon对这些结果感到非常兴奋:“Chopra博士的工作不仅为罹患我这种疾病的人们,也为糖尿病患者找到治疗方法铺平了道路。有机会参与这一过程我感到骄傲和荣幸。”
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
30
#CEL#
26
这是一个很好的开始,二型糖尿病本来胰岛素泛滥,医生还要你打胰岛素。本来患者胰岛功能受损,还吃降糖药,拼命让胰岛细胞生产胰岛素,不死也要让它累死。其实,这根本就不是胰岛素的事。
118
如果真是这样?那么糖尿病有望得到治疗了。患者将会很满意了。期待成功
120
好的发现,期待新的报道
135
静静的等
84
新的进展,值得深入研究
110
文章不错
87
值得关注
90
该文介绍了asprosin在肝糖元释放的G旦白c-AMPPKC通路中的杠杆作用为新药研究指了一亇突破口
88