Neurology:早期治疗动脉瘤可减少aSAH患者住院死亡率
2015-11-24 MedSci MedSci原创
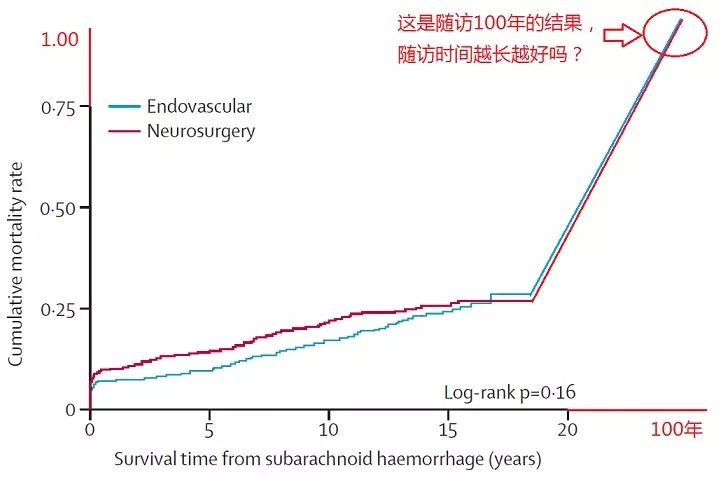
荷兰乌得勒支大学医学院Rudolf Magnus脑中心神经外科Mervyn D I Vergouwen和同事研究动脉瘤性蛛网膜下腔出血后死亡原因的时间变化趋势。研究结果2015年11月20日在Neurology在线发表。早期动脉瘤治疗可减少aSAH住院患者再出血死亡例数,减少住院死亡率。研究结果强调早期闭塞动脉瘤和其他治疗策略减少再出血风险,提高aSAH患者预后的必要性。
荷兰乌得勒支大学医学院Rudolf Magnus脑中心神经外科Mervyn D I Vergouwen和同事研究动脉瘤性蛛网膜下腔出血后死亡原因的时间变化趋势。研究结果2015年11月20日在Neurology在线发表。
目的:比较同一医疗机构中两个时间段因aSAH( aneurysmal subarachnoid hemorrhage ,动脉瘤性蛛网膜下腔出血)住院的患者死亡原因。
方法:前瞻性收集1999-2002年和和2009-2012年844例aSAH发病≤3天内住院的患者数据。评估90天内病死率、住院死亡原因,使用Poisson回归分析计算相对危险度(aRR)和95%CI,以第一时期患者作为对照组,比较患者死亡原因的改变。
结果:1999-2002年aSAH患者90天内病死率是150/381例(39%),2009-2012年aSAH患者90天内病死率下降到140/463例(30%)(aRR0.74,95% CI 0.62-0.88)。
与1999-2002年住院患者特殊死因相比,2009年至2012年住院患者特殊死因中初期出血的aRR为1.06(95% CI 0.72-1.56)、再出血的aRR 0.47(95%CI 0.31-0.71)、迟发性缺血性障碍的aRR 0.91(95%CI 0.50-1.65)。
随着时间推移,住院患者再出血的比例从90/381(24%)下降到78/463(17%)(aRR 0.68,95% CI 0.52-0.90),再出血平均时间从5天(IQR 1-10)下降到0天(IQR 0- 1),动脉瘤治疗平均所需天数从4天(IQR 2-13)下降到1天(IQR 1-2)。
结论:早期动脉瘤治疗可减少aSAH住院患者再出血死亡例数,减少住院死亡率。研究结果强调了早期闭塞动脉瘤和其他治疗策略减少再出血风险,提高aSAH患者预后的必要性。
原始出处:
Mervyn D I Vergouwen, Amy V Jong-Tjien-Fa, Ale Algra, et all. Time trends in causes of death after aneurysmal subarachnoid hemorrhage,A hospital-based study. Neurology. Published online November 20,2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











感觉……这是必然……
83
值得观注
79
非常值得学习,要重视
83
#早期治疗#
55
#ASA#
28
#aSAH#
25
#Neurol#
26
#住院死亡率#
30
#SAH#
34