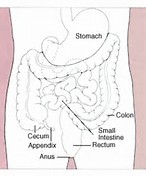
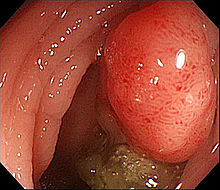
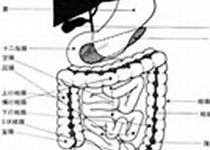
ANN ONCOL:MAPK信号通路基因改变对接受一线FOLFIRI联合贝伐单抗治疗的转移性结直肠癌患者预后的影响
2017-11-08 MedSci MedSci原创
MAPK酶1(MKNK1)位于RAS/RAF/ERK和MAP3K1/MKK/p38信号通路的下游。磷酸化MKNK1调节翻译起始因子4E的功能。翻译起始因子4E是转录控制的关键因素,其表达在转移性结直肠癌患者中升高。临床前数据表明MKNK1上调血管生成因子促进血管生成。ANN ONCOL近期发表了一篇文章,研究MKNK1基因改变是否可以预测接受一线FOLFIRI和贝伐单抗治疗的转移性结直肠癌患者的预
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#患者预后#
0
#基因改变#
40
#MAPK#
39
#Oncol#
45
#转移性#
31
#结直肠#
32
#贝伐#
29
#FOLFIRI#
41
#信号通路#
31