European Radiology:使用表观扩散系数(ADC)直方图分析实现神经母细胞瘤中MYCN扩增的病理级分析!
2022-09-01 shaosai MedSci原创
MYCN扩增可在高达25%的儿童神经母细胞瘤中发现,并可提示患者的预后较差。在任何疾病状态下,MYCN-扩增的存在通常会导致风险类别的上升,因此大大改变了治疗方案,并需要由专门的团队进行进一步治疗。
据统计,神经母细胞瘤是发生在儿童身上的最常见的颅外实体肿瘤。MYCN致癌基因是牵涉到神经母细胞瘤发病机制的几种分子和细胞遗传学途径之一,有助于预测这些肿瘤的临床表现。MYCN致癌基因的过量表达导致MYCN蛋白的产生,这是一种与肿瘤发生有关的转录因子。MYCN扩增可在高达25%的儿童神经母细胞瘤中发现,并可提示患者的预后较差。在任何疾病状态下,MYCN-扩增的存在通常会导致风险类别的上升,因此大大改变了治疗方案,并需要由专门的团队进行进一步治疗。
临床上,通常需要进行开放式或经皮的针式活检来确定神经母细胞瘤的细胞遗传学。这种活检并不理想,由于其只对肿块的一小部分进行取样,而且不同肿瘤部位的基因表达的空间异质性可能会混淆细胞遗传学分析的结果。因此,国际神经母细胞瘤风险小组(INRG)生物学委员会建议,用于细胞遗传学分析的组织应从肿瘤的两个不同区域获得。因此,患者的MYCN扩增状态在最初的活检后可能无法立即得知。
扩散加权成像可对体内质子的随机运动进行量化。恶性肿瘤中细胞的增殖阻碍了质子的自由扩散,被视为扩散受限。组织坏死和肿瘤异质性导致从病变的不同部分获得的ADC值在体素间存在差异,可以通过分析肿瘤中所有ADC值的直方图来进行量化。从ADC直方图分析中得到的指标与各种肿瘤的等级和亚型、预后和治疗结果相关。然而据我扪所知,还没有研究评估ADC直方图分析在确定神经母细胞瘤的MYCN扩增方面的作用。
近日,发表在European Radiology杂志的一项研究评估了整个肿瘤表观扩散系数(ADC)直方图分析在识别神经母细胞瘤MYCN扩增状态中的作用,为术前无创、准确、全面的评估神经母细胞瘤的MYCN扩增状态、进一步实现患者的精准风险分层提供了参考依据。
本研究回顾性地评估了62名神经母细胞瘤患者(中位年龄:15个月(四分位数范围(IQR):7-24个月);38名女性)的影像记录,这些患者在开始任何治疗或活检之前均在本机构接受了磁共振成像检查。14名患者患有MYCN扩增(MYCNA)的神经母细胞瘤。从基线图像和标准化图像中获得整个肿瘤的ADC图的直方图参数。曼-惠特尼U检验用于比较有MYCN扩增和无MYCN扩增的神经母细胞瘤之间的绝对和标准化直方图参数。对于具有统计学意义的直方图参数生成了ROC曲线和曲线下面积(AUC)。从ROC曲线中获得的临界值在外部验证集(n-15,MYCNA-6,F-7,年龄24个月(10-60))上进行了评估。训练了一个逻辑回归模型,通过结合有统计学意义的直方图参数来预测MYCNA,并对验证集进行了评估。
与未扩增的神经母细胞瘤相比,MYCN扩增的神经母细胞瘤具有统计学意义上更高的最大ADC和更低的最小ADC,还表现出比非扩增的肿瘤有更高的熵、方差、能量和更低的均匀性(P>0.05)。能量、熵和最大ADC的AUC分别为0.85、0.79和0.82。

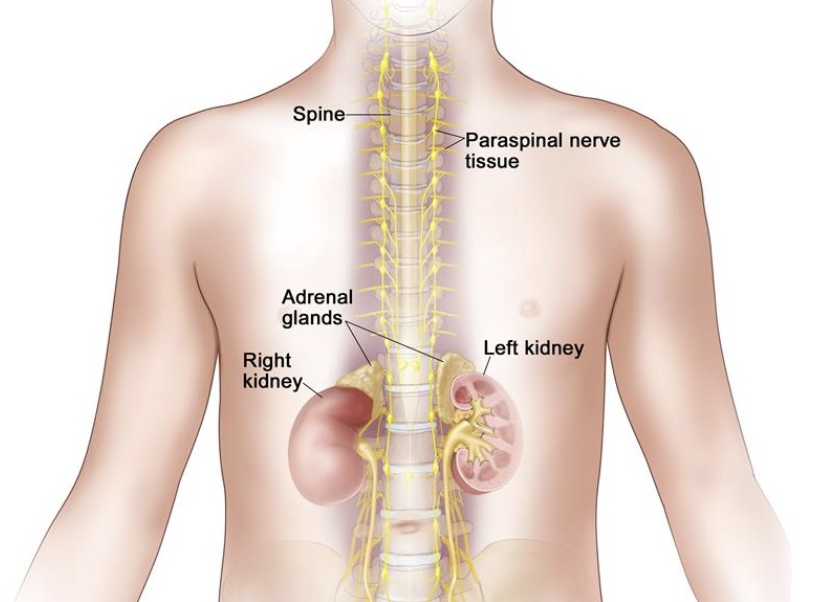
图 肿瘤分割示例:一名6周大的女性患儿,右肾上腺肿块病变和肝转移,为MYNC非扩增型神经母细胞瘤。用低b值图像(A)和ADC图(B)在肿瘤上画出一个3维兴趣区(B和C),然后用它来获得病变的直方图参数(D)
本研究提供了关于ADC直方图参数在预测MYCN-扩增方面的作用的初步回顾性数据。这些参数可以帮助确定定向活检的区域,在活检结果出来之前可以使用这些参数来预测这些高危肿瘤的亚型。
原文出处:
Adarsh Ghosh,Ensar Yekeler,Deepa Dalal,et al.Whole-tumour apparent diffusion coefficient (ADC) histogram analysis to identify MYCN-amplification in neuroblastomas: preliminary results.DOI:10.1007/s00330-022-08750-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PE#
35
#母细胞瘤#
46
#MYCN#
50
#MYC#
68
#细胞瘤#
44