Urol Int:术前睾丸素水平与阳性手术切缘风险正相关关系研究
2018-07-15 AlexYang MedSci原创
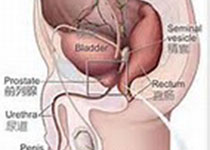
最近,有研究人员在前列腺癌(PCA)中评估了术前总睾丸素(TT)作为阳性手术切缘(PSM)预测因子的情况。研究时间段在2014年11月到2017年7月,在476名PCA且只经历根治性前列腺切除术(RP)的患者中测量了术前TT水平,并且包括了所有风险等级的患者。手术切缘包括阴性、焦点阳性(单个或者小于1ml)和多焦点阳性(多于1个)。研究人员还利用多项逻辑回归模型评估了TT和临床风险因与PSM风险(
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#正相关#
37
#手术切缘#
37
#相关关系#
31
学习了有用的研究
52
学习了谢谢分享
55
#睾丸#
26
#睾丸素#
28
学习了.长知识
60
厉害
55
一起学习学习
51