JACC:动脉粥样硬化性心血管疾病风险预测新指标:胆固醇流出能力
2016-05-27 MedSci MedSci原创
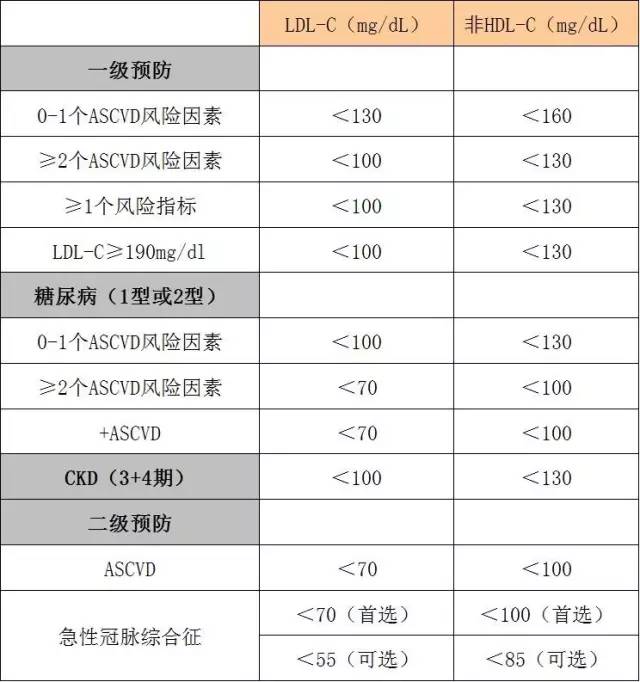
胆固醇流出能力(CEC),这是在胆固醇逆向转运途径的关键一步,与动脉粥样硬化性心血管疾病(ASCVD)独立相关。然而,它是否能超出验证过的新的风险指标来预测ASCVD还是未知的。该研究评估了是否CEC能够超出冠状动脉钙化(CAC),家族史(FH)和高敏C反应蛋白(hs-CRP)的预测能力来改善ASCVD风险预测。研究人员评估了参与者的CEC,CAC,自我报告的FH,和hs-CRP,这些参与者在基线
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
23
#粥样硬化性#
23
#粥样硬化#
22
#动脉粥样硬化性心血管疾病#
25
#ACC#
25
#疾病风险#
30
#风险预测#
23
#硬化性#
31
#血管疾病#
25
#胆固醇流出能力#
31