《动脉粥样硬化性心血管疾病管理血胆固醇治疗亚洲共识》即将发布,一起先睹为快!
2016-05-23 木小一 医学界
《动脉粥样硬化性心血管疾病(ASCVD)管理血胆固醇治疗亚洲共识》即将于2016年5月25日发布! 《ASCVD管理的降胆固醇治疗亚洲共识》中对亚洲患者降胆固醇治疗的推荐囊括六部分,包括改善生活方式、治疗目标、安全性和随访、联合治疗、特殊人群、他汀替代治疗。 改善生活方式和以往变化不大 表1.共识推荐的改善生活方式方案(ABCDE) BMI:体重指数;DASH:终止
《动脉粥样硬化性心血管疾病(ASCVD)管理血胆固醇治疗亚洲共识》即将于2016年5月25日发布!
《ASCVD管理的降胆固醇治疗亚洲共识》中对亚洲患者降胆固醇治疗的推荐囊括六部分,包括改善生活方式、治疗目标、安全性和随访、联合治疗、特殊人群、他汀替代治疗。改善生活方式和以往变化不大
 BMI:体重指数;DASH:终止高血压膳食疗法;MUFA:单不饱和脂肪酸;PUFA:多不饱和脂肪酸
关注!治疗目标值
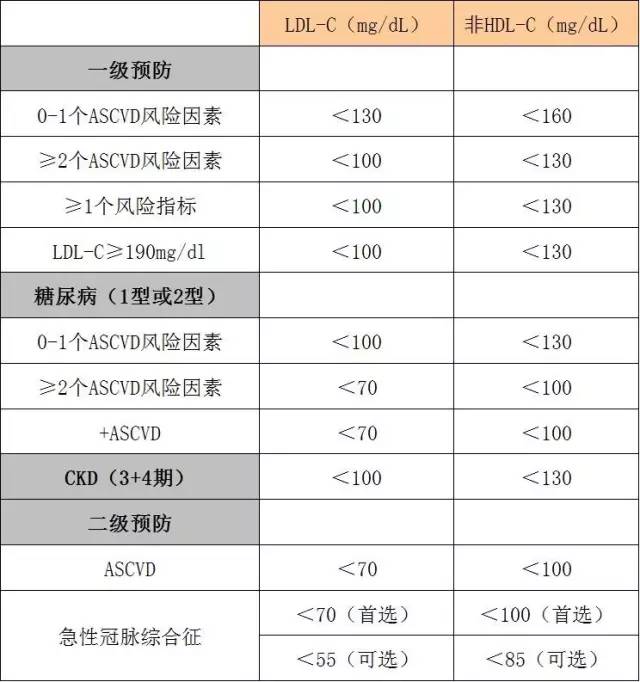
此共识依然坚持降脂目标值观念,原因大致有四点:一是流行病学及随机对照研究显示,降低低密度脂蛋白胆固醇(LDL-C)水平可减少心血管事件;二是治疗后测定LDL-C水平有助于医生确定患者的依从性和他汀不耐受;第三是LDL-C目标有助于患者更好地依从药物治疗和改善生活方式;最后,制定LDL-C目标使联合治疗成为可能。
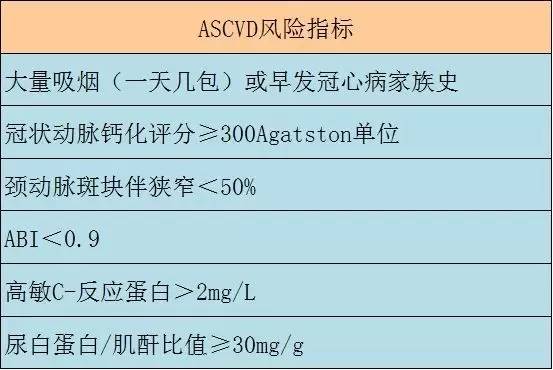
确定治疗目标值的因素包括主要ASCVD危险因素、ASCVD的风险指标、疾病状况(如糖尿病、慢性肾病和ASCVD)以及LDL-C水平。
BMI:体重指数;DASH:终止高血压膳食疗法;MUFA:单不饱和脂肪酸;PUFA:多不饱和脂肪酸
关注!治疗目标值
此共识依然坚持降脂目标值观念,原因大致有四点:一是流行病学及随机对照研究显示,降低低密度脂蛋白胆固醇(LDL-C)水平可减少心血管事件;二是治疗后测定LDL-C水平有助于医生确定患者的依从性和他汀不耐受;第三是LDL-C目标有助于患者更好地依从药物治疗和改善生活方式;最后,制定LDL-C目标使联合治疗成为可能。
确定治疗目标值的因素包括主要ASCVD危险因素、ASCVD的风险指标、疾病状况(如糖尿病、慢性肾病和ASCVD)以及LDL-C水平。
 安全性靠随访及剂量调整
1.他汀的肌肉安全性
RCT显示,他汀治疗后肌痛发生率为1%-5%,常发生在治疗第一个月内,横纹肌溶解是非常罕见的,且肌病与他汀剂量呈正相关。在HPS2-THRIV研究中,与高加索人相比,同等剂量他汀在中国人群中导致了更多肌病,因此中国需要关注辛伐他汀的肌肉安全性问题。当出现他汀相关肌病时,建议再次尝试,对于不能耐受常规剂量他汀的患者,可尝试不同他汀的低剂量治疗。瑞舒伐他汀和阿托伐他汀的半衰期长,适合用于非每日给药治疗。
2.他汀的肝脏安全性
亚洲人群,尤其中国人,因乙肝和脂肪肝的发病率较高,导致肝酶升高的可能性更大。因此,专家组建议仍需要常规监测肝酶。
3.他汀的肾脏安全性
回顾性分析结果显示,与低强度他汀相比,高强度他汀与急性肾脏损害发生率增加相关。但研究可能有许多已知和未知干扰因素以及偏倚因素。
4.他汀相关的癌症
有两者呈相关的研究结果,也有两者不相关的结论。
5.他汀相关的新发糖尿病
一项Meta分析报告显示,他汀使用与新发糖尿病增加9%有关。但他汀对血脂调节的收益依然远大于引起的血糖升高。
6.他汀不耐受
常见他汀不耐受和停药原因包括,肌肉相关不良事件(肌痛、抽筋、乏力)、血清转氨酶水平升高。当肌酸激酶(CK)水平超过10倍正常值上线(ULN)时,应停止他汀治疗。
发生肌肉相关不良事件的患者,可以考虑排除甲状腺和甲状旁腺功能障碍、慢性肾病和电解质异常。
没有证据支持补充维生素D、辅酶Q10用于他汀介导的肌痛和肌病的治疗。
出现他汀不耐受的肌痛或无力时,如何处理呢?首先,停用他汀,经历一个洗脱期;典型症状在数周或数月后缓解;如用药后症状再次出现,证明症状与他汀治疗显著相关,建议转换其他他汀低剂量治疗。
提高依从性仍然很关键
他汀不依从与死亡率、心脑血管事件升高相关。提高依从性需有两个要素,一是简化随访计划和定期血脂检测;二是每次随访时强调长期依从性的重要性及适当的关于降脂对心血管死亡(CV)预后的患者教育。
如果LDL-C和(或)非HDL-C未达到预期水平,应进行依从性评价。有肝功能异常/疾病的患者,接受多种药物治疗或拥有多个医疗服务提供者时,可考虑每6个月随访1次肝功能。
要掌握实现LDL-C目标的三种策略
1.增加他汀剂量。他汀治疗最大程度LDL-C降幅为24%-60%。
2.选择或转换至强效他汀治疗,需考虑降脂幅度和安全性。
3.联合治疗,可与其他降LDL-C药物联合。
总的来讲,《ASCVD管理血胆固醇治疗亚洲共识》有三大亮点:LDL-C治疗达标较他汀剂量更为重要;ACS患者的最佳LDL-C目标可考虑<55mg/dl;证据支持采用联合治疗以达到LDL-C目标值。
共识背景:
近年来,众多学术组织发表了针对高胆固醇血症或血脂异常管理的推荐建议,虽然这些推荐建议存在某些相似性,但也有明显的不同;更重要的是,这些建议中尚无特别针对亚洲人群的推荐。亚洲人群和高加索人群在ASCVD特征、血脂异常特点、药物耐受性等多个方面存在较大差别,欧美指南建议不一定适用于亚洲患者。并且近期发表的多个指南并未纳入遗传学分析数据及最新的临床研究结果。在此背景下,来自亚洲的血脂治疗学者特别成立了专家组,共同讨论、编写针对亚洲人群的血胆固醇管理共识建议。
《动脉粥样硬化性心血管疾病管理血胆固醇治疗亚洲共识》由中国胆固醇教育计划(CCEP)主席、中国老年学学会心脑血管病专业委员会主任委员、我国著名心血管病学家胡大一教授牵头制订,是专门针对亚洲人群而编写的血胆固醇管理建议。国际动脉粥样硬化学会(IAS)主席Philip Barter教授、美国国家脂质学会(NLA)前任主席Peter Toth教授作为顾问参与了共识制订的全过程讨论。来自中国大陆、台湾、香港、日本、韩国的心血管内科、神经内科及内分泌科专家也参与了该共识的讨论制定。
在5月21日的中国动脉硬化性疾病暨中国胆固醇教育计划(CCEP)年年会上,多位专家对即将发布的这一共识的流行病学和循证回顾以及治疗推荐等内容进行了讲解,此文即整理自该会议。
安全性靠随访及剂量调整
1.他汀的肌肉安全性
RCT显示,他汀治疗后肌痛发生率为1%-5%,常发生在治疗第一个月内,横纹肌溶解是非常罕见的,且肌病与他汀剂量呈正相关。在HPS2-THRIV研究中,与高加索人相比,同等剂量他汀在中国人群中导致了更多肌病,因此中国需要关注辛伐他汀的肌肉安全性问题。当出现他汀相关肌病时,建议再次尝试,对于不能耐受常规剂量他汀的患者,可尝试不同他汀的低剂量治疗。瑞舒伐他汀和阿托伐他汀的半衰期长,适合用于非每日给药治疗。
2.他汀的肝脏安全性
亚洲人群,尤其中国人,因乙肝和脂肪肝的发病率较高,导致肝酶升高的可能性更大。因此,专家组建议仍需要常规监测肝酶。
3.他汀的肾脏安全性
回顾性分析结果显示,与低强度他汀相比,高强度他汀与急性肾脏损害发生率增加相关。但研究可能有许多已知和未知干扰因素以及偏倚因素。
4.他汀相关的癌症
有两者呈相关的研究结果,也有两者不相关的结论。
5.他汀相关的新发糖尿病
一项Meta分析报告显示,他汀使用与新发糖尿病增加9%有关。但他汀对血脂调节的收益依然远大于引起的血糖升高。
6.他汀不耐受
常见他汀不耐受和停药原因包括,肌肉相关不良事件(肌痛、抽筋、乏力)、血清转氨酶水平升高。当肌酸激酶(CK)水平超过10倍正常值上线(ULN)时,应停止他汀治疗。
发生肌肉相关不良事件的患者,可以考虑排除甲状腺和甲状旁腺功能障碍、慢性肾病和电解质异常。
没有证据支持补充维生素D、辅酶Q10用于他汀介导的肌痛和肌病的治疗。
出现他汀不耐受的肌痛或无力时,如何处理呢?首先,停用他汀,经历一个洗脱期;典型症状在数周或数月后缓解;如用药后症状再次出现,证明症状与他汀治疗显著相关,建议转换其他他汀低剂量治疗。
提高依从性仍然很关键
他汀不依从与死亡率、心脑血管事件升高相关。提高依从性需有两个要素,一是简化随访计划和定期血脂检测;二是每次随访时强调长期依从性的重要性及适当的关于降脂对心血管死亡(CV)预后的患者教育。
如果LDL-C和(或)非HDL-C未达到预期水平,应进行依从性评价。有肝功能异常/疾病的患者,接受多种药物治疗或拥有多个医疗服务提供者时,可考虑每6个月随访1次肝功能。
要掌握实现LDL-C目标的三种策略
1.增加他汀剂量。他汀治疗最大程度LDL-C降幅为24%-60%。
2.选择或转换至强效他汀治疗,需考虑降脂幅度和安全性。
3.联合治疗,可与其他降LDL-C药物联合。
总的来讲,《ASCVD管理血胆固醇治疗亚洲共识》有三大亮点:LDL-C治疗达标较他汀剂量更为重要;ACS患者的最佳LDL-C目标可考虑<55mg/dl;证据支持采用联合治疗以达到LDL-C目标值。
共识背景:
近年来,众多学术组织发表了针对高胆固醇血症或血脂异常管理的推荐建议,虽然这些推荐建议存在某些相似性,但也有明显的不同;更重要的是,这些建议中尚无特别针对亚洲人群的推荐。亚洲人群和高加索人群在ASCVD特征、血脂异常特点、药物耐受性等多个方面存在较大差别,欧美指南建议不一定适用于亚洲患者。并且近期发表的多个指南并未纳入遗传学分析数据及最新的临床研究结果。在此背景下,来自亚洲的血脂治疗学者特别成立了专家组,共同讨论、编写针对亚洲人群的血胆固醇管理共识建议。
《动脉粥样硬化性心血管疾病管理血胆固醇治疗亚洲共识》由中国胆固醇教育计划(CCEP)主席、中国老年学学会心脑血管病专业委员会主任委员、我国著名心血管病学家胡大一教授牵头制订,是专门针对亚洲人群而编写的血胆固醇管理建议。国际动脉粥样硬化学会(IAS)主席Philip Barter教授、美国国家脂质学会(NLA)前任主席Peter Toth教授作为顾问参与了共识制订的全过程讨论。来自中国大陆、台湾、香港、日本、韩国的心血管内科、神经内科及内分泌科专家也参与了该共识的讨论制定。
在5月21日的中国动脉硬化性疾病暨中国胆固醇教育计划(CCEP)年年会上,多位专家对即将发布的这一共识的流行病学和循证回顾以及治疗推荐等内容进行了讲解,此文即整理自该会议。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#粥样硬化#
27
#疾病管理#
22
#粥样硬化性#
37
#动脉粥样硬化性心血管疾病#
38
#硬化性#
21
#血管疾病#
27