The Oncologist:仑伐替尼联合或不联合依维莫司(Len ±Eve)治疗转移性肾细胞癌(mRCC)的疗效
2021-10-24 yd2015 MedSci原创
研究表明,免疫检查点抑制剂(ICIs)和VEGFR-TKIs联合治疗进展后,仑伐替尼联合或不联合依维莫司(Len ±Eve)治疗转移性肾细胞癌(mRCC)具有一定疗效并且毒性可控。
仑伐替尼 (Len)联合依维莫司(Eve)被批准用于治疗转移性肾细胞癌(mRCC)在一线血管内皮生长因子受体-酪氨酸激酶抑制剂(VEGFR-TKIs)进展后。但是,对于免疫检查点抑制剂(ICIs)和VEGFR-TKIs联合治疗进展后,但关于Len ±Eve的疗效数据有限。因此,来自美国学者开展了回顾性研究,评估免疫检查点抑制剂(ICIs)和VEGFR-TKIs联合治疗进展后,仑伐替尼联合或不联合依维莫司(Len ±Eve)治疗转移性肾细胞癌(mRCC)的疗效。相关结果发表在The Oncologist杂志上。
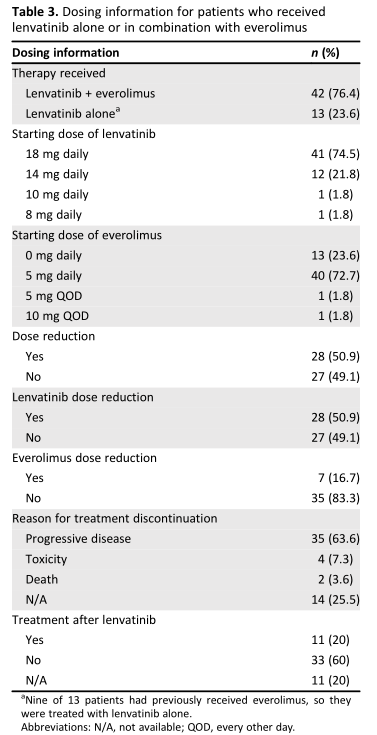
42例(76.4%)患者接受仑伐替尼联合依维莫司治疗,13例(23.6%)患者单独接受仑伐替尼治疗。既往治疗的中位线数为4(范围,2-10线);40%的患者接受仑伐替尼联合或不联合依维莫司作为四线治疗,20%作为五线治疗,16.4%作为六线治疗,16.4%作为七线或以后治疗。所有患者在接受仑伐替尼联合依维莫司或不联合依维莫司之前均接受了ICI, 96.4%的患者接受了舒尼替尼、培唑帕尼或阿昔替尼,83.6%的患者接受了卡博替尼。总之,80%的患者在治疗之前接受了ICI和两种或两种以上VEGFR-TKIs,包括卡博替尼。
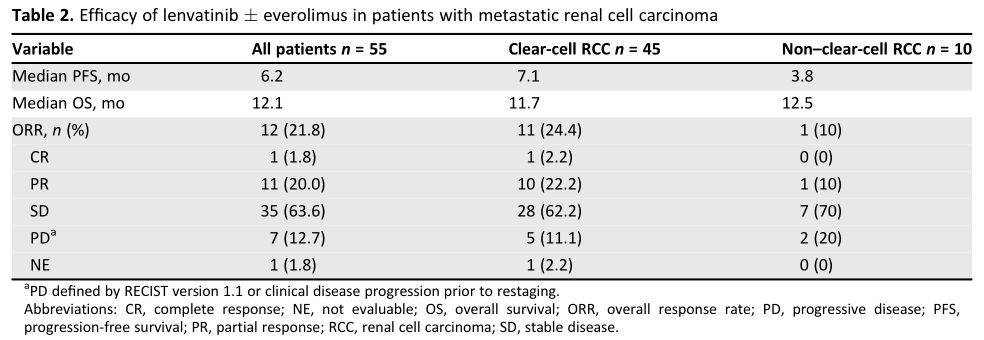
在分析时,48例患者经历了疾病进展或死亡,所有患者的中位无进展生存期(PFS)为6.2个月(95% CI, 4.8-9.4)。ccRCC(肾透明细胞癌)患者的中位无进展生存期为7.1个月(95% CI, 5.0 -10.5), nccRCC(非透明肾细胞癌)患者的中位无进展生存期为3.2个月(95% CI, 3.1- NA)。在分析时,44例患者死亡,所有患者的中位OS为12.1个月(95% CI, 8.8-16.0)。ccRCC患者的中位OS为11.7个月(95% CI, 7.9-16.1), nccRCC患者的中位OS为12.5个月(95% CI, 4.3-NA)。

总体人群PFS和OS
总体人群确认的ORR为21.8%,其中1例患者达到完全缓解(CR)。ccRCC患者的ORR为24.4%,nccRCC患者的ORR为10.0%。在使用仑伐替尼联合依维莫司或不联合依维莫司(n = 46)之前接受ICIs和卡博替尼治疗的患者中(n = 46), ORR为15.2%,67.4%的患者(n = 31)获得病情稳定(SD)。
疗效评估
在13例单独使用仑伐替尼的患者中,9例既往使用过依维莫司,1例既往使用过temsirolimus,因此他们没有再使用依维莫司。绝大多数患者开始时使用仑伐替尼 18 mg /天(74.5%)+依维莫司5 mg /天(72.7%)。50.9%的患者需要减少仑伐替尼的剂量,16.7%的患者需要减少依维莫司剂量。7.3%的患者因蛋白尿和疲劳而停止治疗(各2例)。最常见的3级不良事件是蛋白尿(18.2%)、腹泻(9.1%)和疲劳(9.1%)。没有仑伐替尼或依维莫司相关的4级或5级不良事件。最常见的1 - 2级不良事件是疲劳(67.3%)、恶心(38.2%)、食欲下降(36.4%)、高血压(34.5%)、体重下降(23.6%)和腹泻(21.8%)。
不良事件
综上,研究表明,免疫检查点抑制剂(ICIs)和VEGFR-TKIs联合治疗进展后,仑伐替尼联合或不联合依维莫司(Len ±Eve)治疗转移性肾细胞癌(mRCC)具有一定疗效并且毒性可控。
原始出处:
Wiele AJ, Bathala TK, Hahn AW, Xiao L, Duran M, Ross JA, Jonasch E, Shah AY, Campbell MT, Msaouel P, Tannir NM. Lenvatinib with or Without Everolimus in Patients with Metastatic Renal Cell Carcinoma After Immune Checkpoint Inhibitors and Vascular Endothelial Growth Factor Receptor-Tyrosine Kinase Inhibitor Therapies. Oncologist. 2021 Jun;26(6):476-482. doi: 10.1002/onco.13770. Epub 2021 Apr 21. PMID: 33792094; PMCID: PMC8176993.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
48
#mRCC#
41
#RCC#
43
#细胞癌#
41
#转移性#
0
#转移性肾细胞癌#
47
#GIST#
46