JCO:Ibrutinib治疗慢性淋巴细胞白血病后失败怎么办?抗CD19抗体提供新思路
2017-07-19 xuyihan MedSci原创
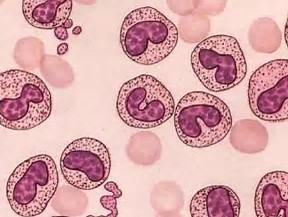
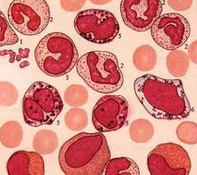
近日在JCO上发表的一篇文章评估了抗-CD19嵌合抗体受体—修饰T(CAR-T)细胞治疗用于先前接受过ibrutinib的慢性淋巴细胞白血病(CLL)患者的安全性和可行性。
近日在JCO上发表的一篇文章评估了抗-CD19嵌合抗体受体—修饰T(CAR-T)细胞治疗用于先前接受ibrutinib的慢性淋巴细胞白血病(CLL)患者的安全性和可行性。
24例CLL患者接受了淋巴细胞化疗和抗-CD19 CAR-T治疗,分为3个剂量水平(2 × 105, 2 × 106 or 2 × 107 CAR-T cells/kg)。19例患者在接受ibrutinib治疗时出现疾病进展,3例患者ibrutinib不耐受,还有2例患者接受ibrutinib治疗时未发生疾病进展。6例患者venetoclax难治,23例有复杂染色体核型和/或17p缺失。
CAR-T细胞灌注后4周,由国际研讨会对慢性淋巴细胞白血病(IWCLL)标准确定的总体反应率(完全反应(CR)和/或部分反应(PR))为71%(17/24)。20例(83%)患者出现了细胞因子释放综合征,8例(33%)患者出现神经毒性,虽然是可逆的但是1例患者出现致命结果。24例中20例接受环磷酰胺和氟达拉滨化疗和CD19 CAR-T细胞达到或者低于最大耐受量(≤2×106 CAR-T cells/kg)。
由此可见,CD19 CAR-T细胞治疗对于接受ibrutinib治疗失败后的高危CLL患者疗效显著。
原始出处:
Cameron J. Turtle.et al. Durable Molecular Remissions in Chronic Lymphocytic Leukemia Treated With CD19-Specific Chimeric Antigen Receptor–Modified T Cells After Failure of Ibrutinib.J CLIN ONCOL.2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#新思路#
27
#淋巴细胞白血病#
23
#JCO#
24
#淋巴细胞#
32
#CD19#
28
#ibrutinib#
35