JCC: 前瞻性研究证实肉类摄入与溃疡性结肠炎的高风险相关
2022-09-13 xuyihan MedSci原创
炎性肠病又称炎症性肠病(IBD),为累及回肠、直肠、结肠的一种特发性肠道炎症性疾病。临床表现腹泻、腹痛,甚至可有血便。本病包括溃疡性结肠炎(UC)和克罗恩病(CD)。
在20世纪,尤其是在下半叶,北美和欧洲的炎症性肠病[IBD]发病率有所增加。最近,在以前不受IBD影响的新兴工业化国家,如亚洲、中东和南美,IBD的发病率也有所增加。这些时间趋势表明环境因素在IBD病因中的作用。工业化与许多生活方式的改变有关,包括城市化、医疗保健、抗生素的广泛使用、暴露于不同类型的环境污染、缺乏运动和西方饮食。因此,更好地了解导致全球IBD发病率增加的驱动力可能有助于制定预防策略。这些都是必要的,特别是在印度和中国等亚洲大国,预计在接下来的几十年中,IBD 患者的数量将不断增加。
之前有两项研究调查了蛋白质摄入与IBD风险之间的关系,然而,这些研究仅限于单一性别或相对较少的IBD病例。在最近对IBD环境风险因素荟萃分析的综合审查中,发现蛋白质摄入与IBD之间关联的可信度很弱。因此,本项研究试图在欧洲癌症和营养前瞻性调查 [EPIC] 中调查蛋白质和蛋白质摄入来源与IBD风险之间的关联。
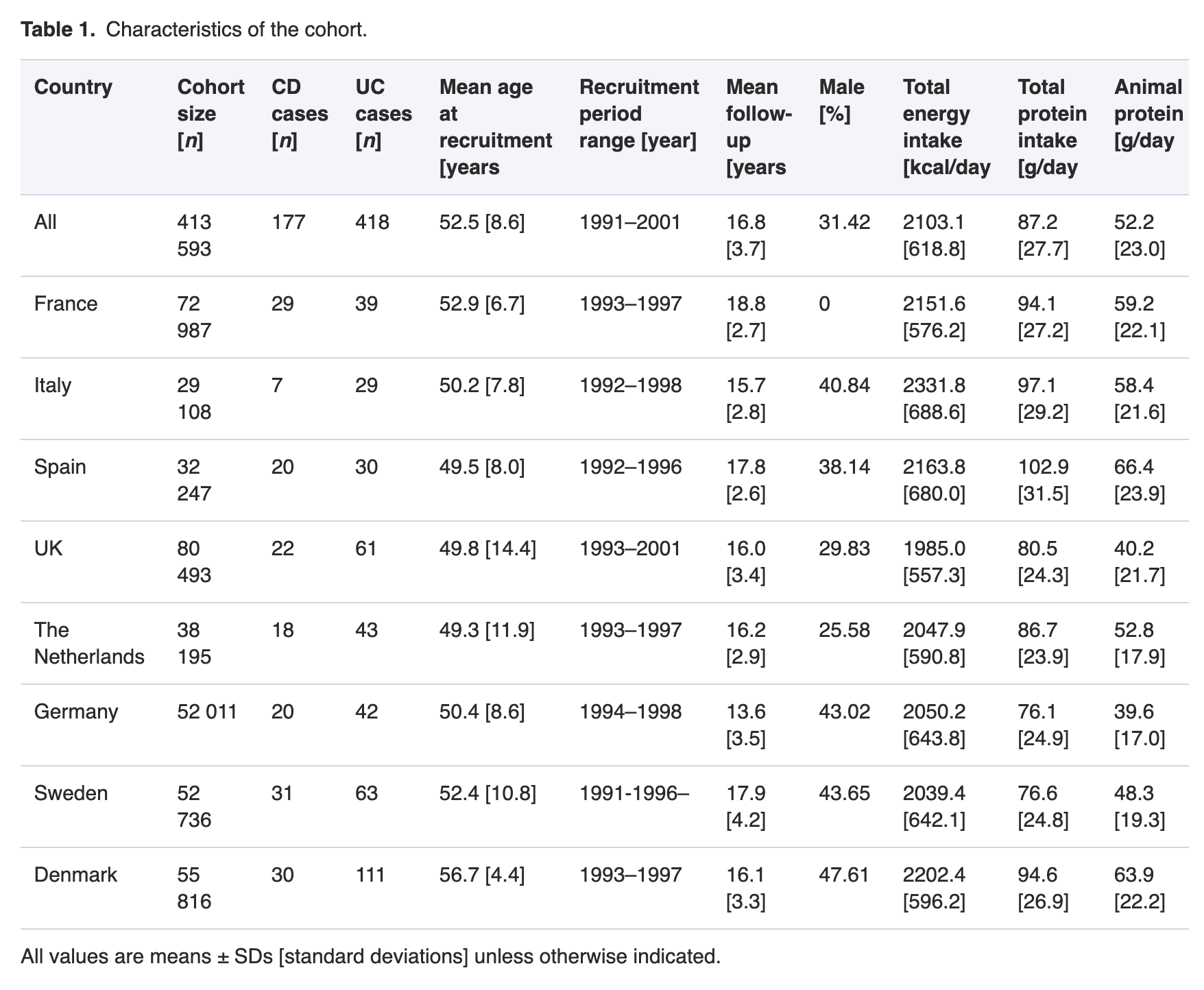
本项研究共有来自八个欧洲国家的413593名参与者。饮食数据是从经过验证的食物频率问卷中收集的。膳食数据经过研究人员的校准,以纠正与每个国家特定问卷相关的措施中的偏倚。通过Cox比例风险模型估计蛋白质 [总、动物和蔬菜] 或动物蛋白质的食物来源与 IBD 风险之间的关联。
研究结果显示平均随访16年后,共有177名克罗恩病 [CD] 患者和418名溃疡性结肠炎 [UC] 患者被纳入分析。总蛋白、动物蛋白或植物蛋白摄入量与CD或UC风险之间没有关联。肉类和红肉总摄入量与UC风险相关(第 4 与第 1 个四分位数的风险比 [HR] = 1.40,95% 置信区间 [CI] = 0.99-1.98,p=0.01;和 1.61,95% CI = 1.10-2.36, p=0.007]。动物蛋白的其他食物来源[加工肉、鱼、贝类、蛋、家禽]和UC之间没有关联。但是研究人员没有发现动物蛋白的食物与CD之间存在风险关系。
本项研究证实肉类和红肉消费与更高的UC风险相关。这些结果支持对IBD高危人群的肉类摄入进行饮食咨询以减少疾病发生概率。
原始出处:
Catherine Dong. et al. Meat Intake Is Associated with a Higher Risk of Ulcerative Colitis in a Large European Prospective Cohort Study. Journal of Crohn's and Colitis.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#前瞻性研究#
44
#溃疡性#
42
#高风险#
49
#前瞻性#
53