
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
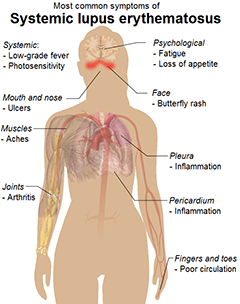


系统性红斑狼疮(SLE)是一种病因不明的异质性自身免疫性疾病。患者可表现为相对良性的病程或急进而严重的病程,甚至导致器官衰竭乃至死亡。SLE主要在20或30多岁的女性人群中发病,但其性质和严重程度会因年龄而异。疾病的严重程度和临床表现在“早发组”和“迟发组”会有不同。 一些队列研究专门研究'“迟发性SLE”。其定义为50岁后确诊为SLE的患者。据报道“迟发组”与年轻的
关节表现常常是系统性红斑狼疮(SLE)患者最常见和最早出现的临床症状。临床判断SLE的关节病变常应用ACR非侵蚀性关节炎的诊断标准,但SLE也有非侵蚀性变形性关节炎(Jaccoud关节)和伴关节侵蚀畸形的关节炎(Rhupus综合征)。而目前对SLE关节炎的研究却较少。 为了探讨核磁共振(MRI)在SLE关节炎的诊断价值和SLE关节炎的临床特点,爱尔兰的Ball教授等做了一项病例对照研究,
由中科院上海药物研究所左建平研究组与李英研究员历时15年研发的治疗系统性红斑狼疮的1.1类候选新药“马来酸蒿乙醚胺”日前获国家食品药品监督管理总局(SFDA)核准的I、II、III期临床研究批件,即将启动临床研究。系统性红斑狼疮(SLE)是一种难治的自身免疫性疾病,临床上长期缺乏新型治疗药物。目前SLE临床治疗仍然以糖皮质激素为基础,联合使用非特异性抗炎、免疫抑制剂,但长期使用易造成免疫功能低下等
为了评估系统性红斑狼疮(SLE)患者临床骨折风险,并评估SLE患者临床骨折相关的危险因素,来自英国南安普顿大学附属南安普顿总医院的F. de Vries教授及其团队进行了一项研究,该研究发现SLE患者临床骨折风险增加,之前6月内使用糖皮质激素、病程长伴有神经、精神系统损伤和之前有骨质疏松性骨折病史与SLE患者骨折风险增加有关。该研究结果在线发表在2013年12月03日的Os
研究要点: 1.系统性红斑狼疮患者的抑郁症患病率显著高于一般人群。 2.患者抑郁评分分数与疾病严重程度无关。 3.系统性红斑狼疮患者伴发抑郁症时治疗率低,应引起重视并进行积极治疗。 目前评估系统性红斑狼疮(SLE)与抑郁症的患病率之间关系的研究较少,一些研究中报道,SLE患者抑郁症患病率为23%—55%,但这些研究的数据都未与一般人群的抑郁症患病率作比较,且已出版的研究中亦无评估心理应激与
系统性红斑狼疮(SLE)是一种慢性炎症性多系统疾病,肌肉骨骼系统病变是该疾病最常出现的症状之一,同时也可能是最早出现的症状。SLE的关节受累表现为关节痛、关节炎以及少见的关节畸形。来自意大利罗马第一大学的Iagnocco博士等对SLE患者的关节病变进行了一项临床研究。 研究者对SLE患者的手、腕、足关节进行超声(US)检查,评估局部炎症性病变的发病率与严重性,并将检查结果与患者的临床症状、实验室


梅斯医学MedSci APP
医路相伴,成就大医
多浆膜腔积液和血液系统损害也是常见表现
54
#系统性#
34
看看
106
图文学起来就是容易得多!
159
只见于女性吗?
116
#狼疮#
31
#红斑#
23
好东东
97
画的图不错
89
挺好
64