JCC: 治疗早期肠道超声检查结果可预测克罗恩病抗 TNFα 治疗的内镜反应
2022-07-12 xuyihan MedSci原创
克罗恩病是一种慢性的肠道炎症,可以从口腔、肛门、全消化道发生,往往最为常见的好发部位是在回盲部以及小肠,它的主要临床表现是腹痛、腹块、瘘管形成、肠梗阻。
克罗恩病 [CD] 是一种慢性炎症性疾病,可影响整个胃肠道,在CD的治疗中,在治疗环境中进行密切监测是预防复发和并发症的关键原则。尽管临床症状的存在可能反映活动性炎症,但临床评分指标与疾病活动的真实状态相关性较差;因此,需要采取其他客观措施。内窥镜检查已成为客观化活动性炎症的金标准。
然而,它是侵入性的、昂贵的费用使得它并没有成为一个有吸引力的工具,肠道超声 [IUS] 是一种有前途的非侵入性横断面成像技术,具有低成本和高可及性。
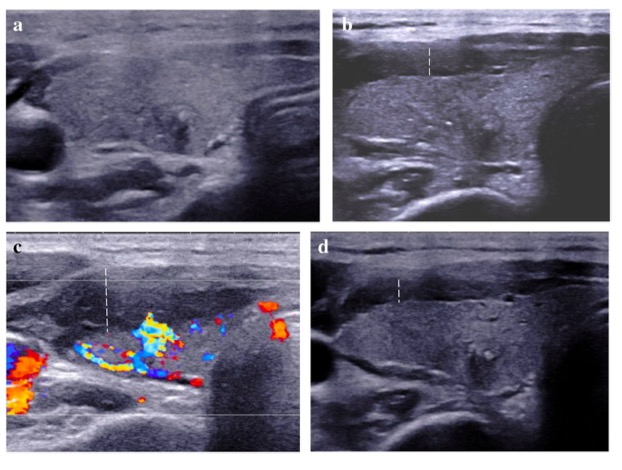
以前的研究表明,与内窥镜检查或磁共振成像 [MRI] 相比,IUS 检测疾病活动、严重程度和范围的准确性很高。除了B模式和多普勒参数外,还研究了对比增强超声 [CEUS]。CD中的炎症导致微血管密度增加和GI壁局部血流失调。这会导致肠壁灌注的变化,这可以通过 CEUS 进行量化。以前的研究表明,CEUS 在内窥镜检查中确定疾病活动以及预测早期内窥镜反应和缓解方面的作用,因此,本项研究旨在探究IUS和对比增强超声 [CEUS] 预测内镜治疗反应的能力。
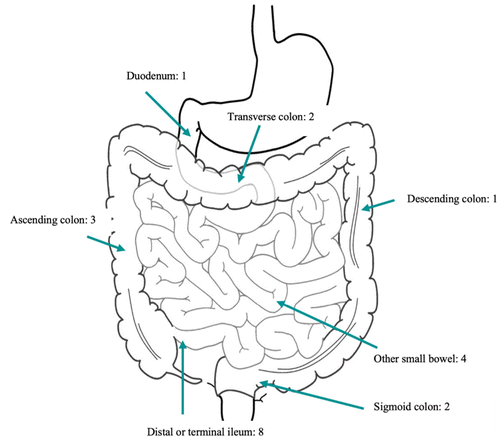
本项研究纳入了包括内镜下活动性CD患者,所有患者均开始抗TNFα治疗。研究人员同时收集患者基线 [T0]、4-8 周 [T1] 和12-34周[T2]后的临床、生化、IUS和CEUS数据。确定了内窥镜检查中炎症最严重的节段(克罗恩病的最高节段简化内镜评分 [SES-CD])和 IUS(最高节段肠壁厚度 [BWT])。在 T2 时,对内镜反应 [SES-CD 减少 ≥ 50%] 和缓解 [SES-CD=0] 进行评分。
本项研究共纳入40名患者:14名达到内镜缓解,17名出现内镜下复发。最高节段肠壁厚度 [BWT]在内镜下缓解的患者中明显较低 T1 (3.1 mm [1.9–4.2] vs 5.3 mm [3.8–6.9], p = 0.005) 和 T2 (2.0 mm [1.8–3.1] vs 5.1 [3.0–6.3] mm, p= 0.002) 。最高节段肠壁厚度 [BWT]越高对于预测内窥镜反应越差:T1和T2时,18%(受试者工作曲线下面积 [AUROC]:0.77;优势比 [OR]:10.80,p= 0.012)和 29% [AUROC:0.833;OR:37.50,p= 0.006]。为了确定内镜缓解,BWT为 3.2 mm是最准确的截断值 [AUROC:0.94,p< 0.0001]。

本项研究证实在4-8 周的随访中,BWT的降低预测了内镜反应和缓解。CEUS 参数的价值有限。此外,本项研究还提供了 BWT 在不同时间点反映内窥镜反应和缓解的准确截止值。
原始出处:
F de Voogd. Et al. Intestinal Ultrasound Early on in Treatment Follow-up Predicts Endoscopic Response to Anti-TNFα Treatment in Crohn’s Disease. Journal of Crohn's and Colitis.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TNFα#
51
#检查结果#
43
学习了
41
#内镜#
51
#超声检查#
45
#TNF#
34