半月板同种异体移植的长期软骨保护作用:一项 10 至 14 年的随访研究
2022-01-16 MedSci原创 MedSci原创
半月板异体移植(MAT)的长期软骨保护作用及其对半月板切除术的优越性鲜有报道。
半月板异体移植(MAT)的长期软骨保护作用及其对半月板切除术的优越性鲜有报道。
在此,研究者提出一个假设,并就此开展队列研究,即与半月板缺失的膝关节相比,MAT会减少骨关节炎(OA)的进展。移植物的挤压距离将强烈影响MAT的软骨保护作用。

图1文章来源
该研究共有17个接受MAT的膝关节作为MAT组进行随访。根据磁共振成像(MRI)冠状切面上3毫米的挤压情况,MAT组被进一步分为非挤压亚组(n = 9)和挤压亚组(n = 8)。
另有26名在同一时期接受半月板切除术的连续患者作为ME组进行随访。健康对照组包括从MAT和ME组中选择的健康对侧腿(n = 27)。
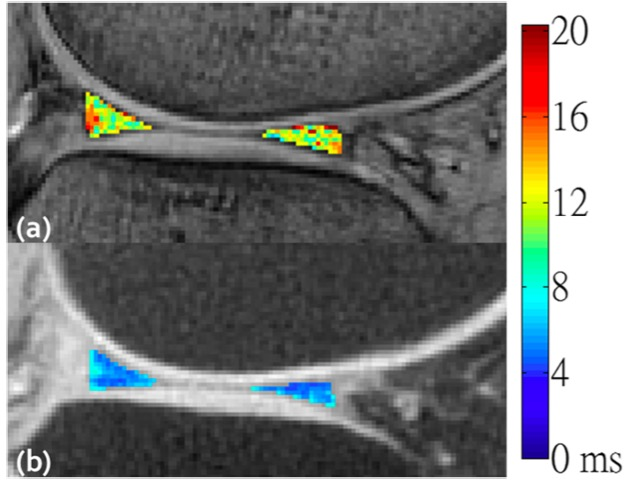
关节间隙宽度(JSW)在X光片上被测量。使用T2映射序列的三维MRI定量分析软骨变性和半月板异体移植在5个方向(0°、45°、90°、135°和180°)的挤出情况。根据MRI扫描中软骨病变的大小和程度,计算软骨变性指数(CDI)。分析了CDI增加与挤压距离之间的相关性。
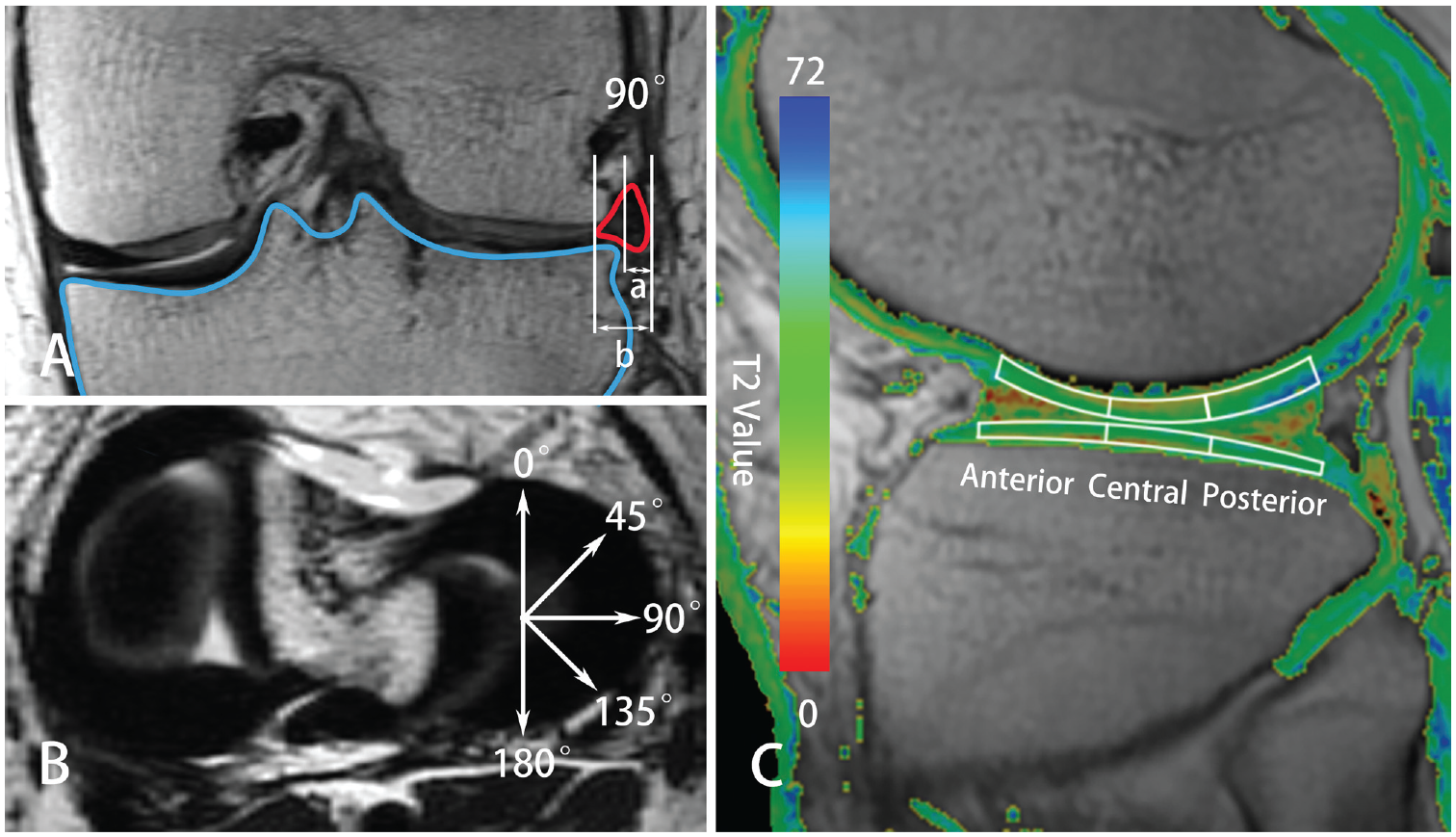
图2(A,B)通过3维磁共振成像在5个径向测量绝对距离(a)和相对挤压百分比(a/b ×100%)。(C) T2 映射序列上的感兴趣区域。测量中央负重部位软骨的T2值。
结果显示,平均随访时间为11.3年(范围为10-14年)。
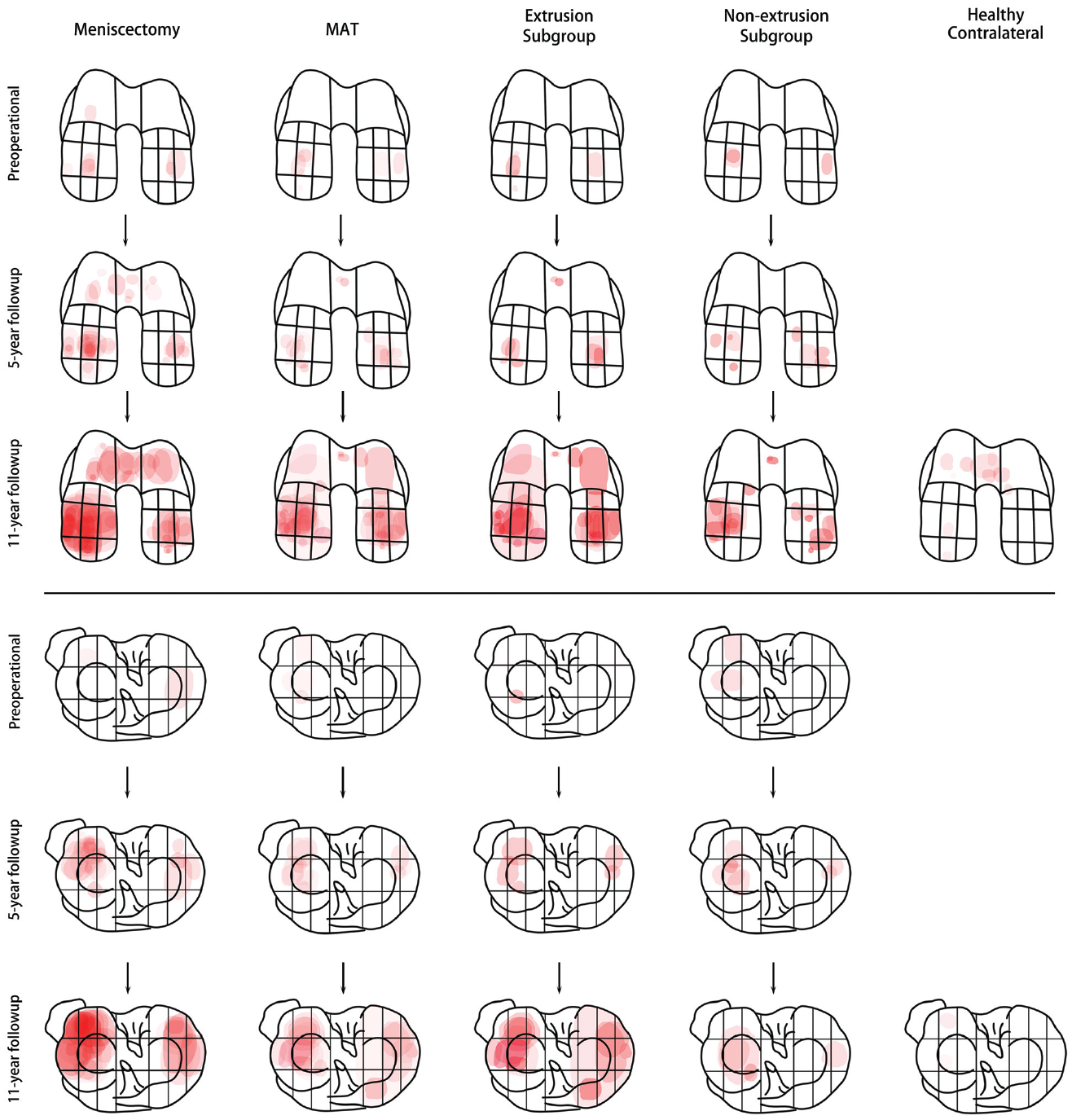
图3 半月板同种异体移植 (MAT) 组、MAT 非挤压亚组、MAT 挤压亚组和半月板切除术组(红色区域)中股骨和胫骨软骨的软骨病变进展。总体而言,与半月板切除术相比,MAT 在长期软骨保护方面具有中等优势。非挤压半月板的软骨保护作用接近于天然半月板,而挤压> 3 mm的同种异体半月板完全失去其功能,与半月板切除术相同
与ME组相比,MAT组在软骨保护方面具有中度优势,JSW变窄(0.58±0.66毫米)和CDI增加(1132±1589)较少(JSW变窄。1.26 ± 1.13 mm, P = .025; CDI增加。2182 ± 1958, P = .079).
挤压组的JSW变窄(0.71±0.80mm;P=0.186)和CDI增加(2004±1965;P=0.830)与ME组接近,表明3mm的挤压导致半月板软骨保护作用完全丧失。
非挤压组的JSW变窄(0.48±0.48mm;P=0.042)和CDI增加(358±249;P=0.011)明显少于ME组。
健康对照组的JSW变窄为0.22±0.27毫米。挤压亚组的软骨T2值与ME组相似,有更多的OA特征,而非挤压亚组的T2值则更接近健康对照组。
在多变量回归模型中,90°方向的挤压距离(P=0.002)和随访时间(P=0.019)显著影响CDI的增加。与其他单个方向相比,45°、90°和135°方向的平均挤压距离能更好地预测软骨保护作用。
综上述,从长远来看,与半月板切除术相比,MAT在长期的软骨保护方面有一定的优势。移植物的挤压距离强烈影响MAT的软骨保护效果。无挤压的半月板异体移植的软骨保护作用接近于原生半月板,而挤压大于3mm的异体移植在半月板切除后完全失去了功能,类似于半月板切除术。
原始文章:
Wang DY, Zhang B, Li YZ, Meng XY, Jiang D, Yu JK. The Long-term Chondroprotective Effect of Meniscal Allograft Transplant: A 10- to 14-Year Follow-up Study. Am J Sports Med. 2022 Jan;50(1):128-137. doi: 10.1177/03635465211054022. Epub 2021 Nov 19. PMID: 34797194.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#同种异体#
37
#随访研究#
32
#半月板#
37
#异体移植#
34
#保护作用#
36