BJD:天疱疮治疗新靶点:BTK抑制剂
2022-02-07 医路坦克 MedSci原创
寻常型天疱疮(PV)是一种罕见的破坏性自身免疫性大疱性疾病。研究证明利扎布替尼(BTK抑制剂)可以作为治疗这种严重、难治性疾病的新口服药物。

寻常型天疱疮(PV)是一种罕见的破坏性自身免疫性大疱性疾病。直到最近,治疗还需要大剂量口服皮质类固醇和非靶向免疫调节剂,如静脉注射免疫球蛋白(IVIG)、硫唑嘌呤、霉酚酸酯和环磷酰胺。利妥昔单抗是一种抗CD20的单克隆抗体,它通过消耗B细胞来发挥作用,使PV的治疗发生了革命性的变化。利妥昔单抗可以诱导40%的患者长期缓解皮质类固醇激素,而霉酚酸酯的这一比例为10%。利妥昔单抗是一项突破,它改善了结果,减少了IVIG的使用率。然而,仍然需要安全有效的治疗来优化PV患者的预后。在本期《英国医学杂志》上,Murrellet al。Bruton酪氨酸激酶(BTK)抑制剂rilzabrutinib治疗PV的早期发现。
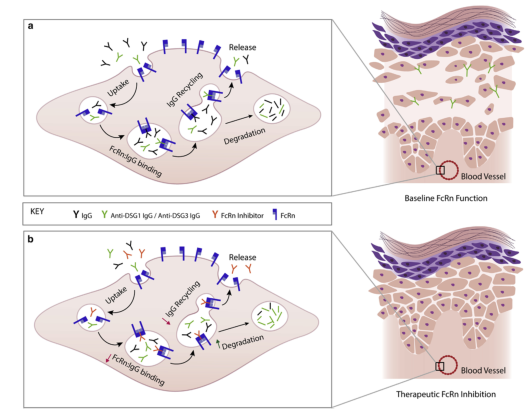
利扎布替尼( Rilzabrutinib)和利妥昔单抗一样,通过靶向B细胞发挥作用。在PV中,异常的B细胞会产生针对桥粒蛋白1和3的抗体,这两种蛋白对角质形成细胞的黏附非常重要。BTK对B细胞的增殖、分化和生存至关重要,使其成为PV治疗的一个有吸引力的靶点。
在一项II期试验中,患有中到重度PV的成年人每天口服利扎布替尼400 mg,持续12周。患者每天服用相当于泼尼松的0.5mgkg-1的口服皮质类固醇,并允许更大剂量的激素进行抢救。如果患者能够控制疾病活跃度(CDA),即所有天疱疮皮损愈合并且没有新的皮损发展,皮质类固醇激素就会逐渐减少。
接受利扎布替尼治疗的患者中有一半(14/27)在4周时达到主要终点,即CDA,口服皮质类固醇剂量维持在每日0.5mgkg-1以下。值得注意的是,主要结果的评估是在非常短的终点(4周)进行的,这表明对一些患者来说,利扎布替尼是快速有效的。再服用利扎布替尼8周后,CDA发生率提高到70%。在总共治疗12周后,利扎布替尼被停用,在12周的非治疗期结束时,CDA率继续改善,最高可达85%,这表明利扎布替尼可能有较长的疗效。
这些结果是有希望的,研究人员为罕见和严重的疾病提供了高质量的数据,应该受到赞扬。尽管如此,仍需要进行对照研究,特别是与利妥昔单抗等活性对照药物的对照研究。虽然在4-12周内实现天疱疮控制的患者数量令人印象深刻,但口服皮质类固醇剂量的减少并不是特别显著。初诊天疱疮患者12周内平均皮质类固醇剂量由20 mg/d降至11.8 mg/d,复发性天疱疮患者仅由10.3 mg/d降至7.8 mg/d。
总而言之,天疱疮患者和治疗他们的皮肤科医生应该对利扎布替尼持谨慎乐观态度,更广泛地说,应该将BTK抑制剂作为治疗这种严重、难治性疾病的新口服药物。我们期待看到正在进行的III期安慰剂对照试验的结果;每天5毫克或更少剂量的泼尼松完全缓解的初步结果将为患者、临床医生和调节者评估利扎布替尼在PV治疗中的作用提供非常有意义的信息。
文献来源:Drucker AM, Shear NH,Bruton tyrosine kinase inhibition warrants further study for pemphigus.Br J Dermatol 2021 10;185(4)

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#抑制剂#
39
好好
46
#新靶点#
29
#BTK抑制剂#
43
#治疗新靶点#
41
#BTK#
36