纳米仿生,植骨支架材料研究的新思路
2017-06-02 伊文 MaterialsViews
骨缺损的再生与修复一直是医学界的难题。骨植入品可以帮助新骨的愈合以及作为替代材料植入骨缺陷处。市面上的自体移植物由于供体部位的病态,异基因移植物由于免疫排斥、病毒的传输以及合成移植物由于生物活性的不足,不能很好地满足临床的需求。因此生物相容性优越、成骨性能良好、降解速度适宜的骨替代材料的研发一直是研究的热点与难点。然而,传统的骨组织工程支架材料仅仅是对天然骨化学组成的简单模仿,并未再现天然骨组织的
骨缺损的再生与修复一直是医学界的难题。骨植入品可以帮助新骨的愈合以及作为替代材料植入骨缺陷处。市面上的自体移植物由于供体部位的病态,异基因移植物由于免疫排斥、病毒的传输以及合成移植物由于生物活性的不足,不能很好地满足临床的需求。因此生物相容性优越、成骨性能良好、降解速度适宜的骨替代材料的研发一直是研究的热点与难点。然而,传统的骨组织工程支架材料仅仅是对天然骨化学组成的简单模仿,并未再现天然骨组织的多级结构。
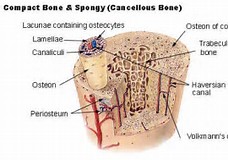
近日,中国科学院化学研究所王铁研究员课题组和北大口腔周彦恒课题组合作研究提出了一种新的解决方案,从纳米级别对天然骨组织的各级结构进行仿生合成,制备了具有良好的生物相容性及生物活性,能诱导内源性骨再生的骨替代材料—拓扑结构的纤维内矿化胶原(Hierarchical intrafibrillarly-mineralized collagen,HIMC)。为了体外再现生物体内的矿化过程,本研究使用改良的“自下而上”仿生矿化法实现三维的HIMC支架的合成。研究表明,仿生合成的HIMC支架材料具有于天然骨极其相似的纳米结构,能够更好的促进干细胞在支架材料表面的粘附、增殖与矿化;且与天然骨具有类似的应力分散能力及降解速率;体内研究表明在HIMC支架材料引导下生成的新骨量更高,分布广泛,纳米结构更成熟,尤其是新生骨胶原与天然骨胶原的排列及机械性能一致。目前,纤维内矿化胶原支架材料的研发取得了阶段性的进展,相信在不久的将来会为骨缺损的临床治疗提供新思路。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#新思路#
21
#支架材料#
37
#骨支架#
27
#骨支架#
35