The Lancet:组织工程化气管移植术是一种安全且有前途的新技术
2013-10-23 sd3212 dxy
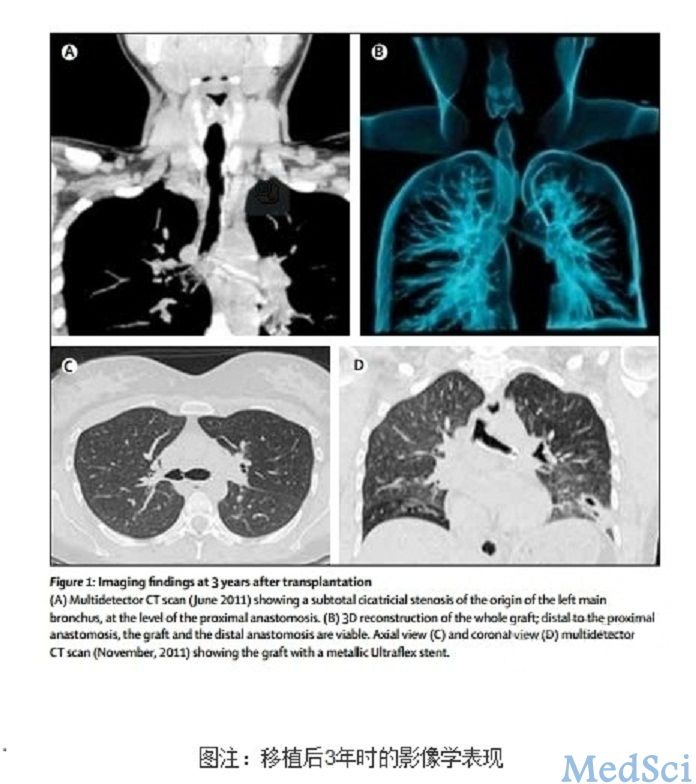
(A) 2011年六月,多排螺旋CT扫描显示:左侧主支气管根部、近吻合口处几乎呈完全性瘢痕性狭窄;(B)整个移植物从远端到近端的三维重建显示:整个移植物及远端吻合口通常;(C)、(D)2011年11月,轴位和冠状位多排CT扫描显示的移植物、及UltraFlex金属支架。2008年,一位晚期左主支气管软化患者接受了人类首次组织工程化气管移植手术。当时,接受手术的这位女性患者只有30岁。近日,来自瑞典
(A) 2011年六月,多排螺旋CT扫描显示:左侧主支气管根部、近吻合口处几乎呈完全性瘢痕性狭窄;(B)整个移植物从远端到近端的三维重建显示:整个移植物及远端吻合口通常;(C)、(D)2011年11月,轴位和冠状位多排CT扫描显示的移植物、及UltraFlex金属支架。【原文下载】
2008年,一位晚期左主支气管软化患者接受了人类首次组织工程化气管移植手术。当时,接受手术的这位女性患者只有30岁。近日,来自瑞典胡丁厄市卡罗林斯卡学院耳鼻喉科、当代移植与再生医学中心的Paolo Macchiarini及其同事总结了该患者术后5年的随访结果,其随访报告在线发表于2013年10月23日的《柳叶刀》(the lancet)杂志上。报告显示:组织工程化气管移植术、包括人类气管脱细胞技术、自体上皮细胞及干细胞培养和分化技术、细胞“脚手架”播种技术等组织工程技术是一类安全、且有前途的新技术。
研究者大约每3个月对患者进行一次多排螺旋CT扫描及支气管镜评估随访;每6个月进行一次粘膜活检标本组织学、免疫组织化学、和电子显微镜方面的检查评估。此外,研究者还对患者的生活质量、呼吸功能、咳嗽反射试验、以及患者体内抗供体人类白细胞抗原抗体的产量及其特异性等进行了随访评估。
该研究的主要结果为:至移植术后第12个月时,接近组织工程化气管吻合口处的宿主气管已出现了渐进性的瘢痕狭窄,为此,患者需要反复进行腔内支架置入术,以延缓狭窄的进展。然而,置入的组织工程化气管本身仍然保持全长通畅、血供良好;而且宿主的呼吸道上皮细胞已经对其完成了全部的重新上皮化,并使之具备了正常的纤毛运动、及粘液清除功能。患者的肺功能和咳嗽反射均正常。随访未发现与干细胞有关的畸胎瘤形成,也未发现有抗供体抗体产生。除了需要进行间断性的支气管镜介入检查及治疗外,患者的社会和工作生活均正常。
该研究结果显示:组织工程技术是一类安全、且有前途的新技术。而人类气管脱细胞技术、自体上皮细胞及干细胞培养和分化技术、以及在生物反应器内进行的细胞“脚手架”播种技术等,也均包含在这一类技术之列。
原文出处
Alessandro Gonfiotti, Massimo O Jaus, Daniel Barale, Silvia Baiguera , Camilla Comin, Federico Lavorini, Giovanni Fontana , Oriol Sibila , Giovanni Rombolà Philipp Jungebluth , Prof Paolo Macchiarini.The first tissue-engineered airway transplantation: 5-year follow-up results.The Lancet 2013 Oct 23【原文下载】
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
18
#移植术#
32
#新技术#
29
#组织工程#
23