Spine :颈前路减压融合术后脑脊液漏的处理策略
2014-09-12 黄稳定 丁香园
颈前路减压融合术(ACDF)是治疗颈椎疾患常用的手术方式,如神经根型颈椎病、颈椎管狭窄、脊髓型颈椎病、颈椎不稳或创伤等。该术式手术效果较好,并发症及死亡率发生率低,而且并发症通常比较轻。 ACDF术后并发症包括:术后血肿、吞咽困难、喉返神经麻痹、食管穿孔、Horner综合征、症状加重及伤口感染等。早期重视ACDF术后并发症可以有效减少对预后的影响,提高临床治疗效果。 脑脊液漏是颈前路术后一种少
颈前路减压融合术(ACDF)是治疗颈椎疾患常用的手术方式,如神经根型颈椎病、颈椎管狭窄、脊髓型颈椎病、颈椎不稳或创伤等。该术式手术效果较好,并发症及死亡率发生率低,而且并发症通常比较轻。
ACDF术后并发症包括:术后血肿、吞咽困难、喉返神经麻痹、食管穿孔、Horner综合征、症状加重及伤口感染等。早期重视ACDF术后并发症可以有效减少对预后的影响,提高临床治疗效果。
脑脊液漏是颈前路术后一种少见但较为严重的并发症,但是具体的发病率与脑脊液漏的具体定义相关,文献报道认为其发病率为0.2%-0.5%,而颈前路OPLL手术后脑脊液漏的发生率较高,达到了4.3%-32%。
文献上有关ACDF术后脑脊液漏的发病率、临床表现及治疗的论文均较少,主要原因有发病率低、发表性偏倚以及对该并发症估计不足。与腰椎手术不同的是,由于手术野较小,操作空间有限,而且紧贴脊髓,因而前路手术引起的脑脊液漏则很难从根本上进行修复。绝大多数ACDF手术引起的脑脊液漏是在术中发现并确诊,但是,一些微小的裂口则不易被发现,尤其是在蛛网膜保持完整、没有明显的脑脊液漏发生的情况下;这些隐秘的脑脊液漏则发生较晚,通常在术后表现为脑脊液从伤口渗出,甚至出现脑膜炎(颅内感染)、伤口周围肿胀、颈部肿块等严重症状。
美国学者Syre等对ACDF术后因硬膜囊撕裂而导致的脑脊液漏的病例进行了随访,并对文献进行了总结回顾,提出了ACDF术后脑脊液漏的治疗策略,其研究结果发表在最新一期的Spine杂志上。
作者对2000-2011年间在宾夕法尼亚医院和长老会医院手术的患者进行回顾性分析,患者的纳入标准如下:(1)年龄≥18岁;(2)接受ACDF手术者;(3)术后出现脑脊液漏。OPLL患者则被排除在研究之外。脑脊液漏的诊断标准:(1)术中见到脑脊液溢出,无论量有多少;(2)术后见脑脊液从伤口内渗出;(3)影像学确认脑脊液局部集聚。作者对患者的住院记录、临床诊治记录、影像学资料、麻醉记录以及手术记录等进行回顾性分析。
根据这些记录,可以确定患者的年龄、性别、手术方式、脑脊液漏发生和治疗的过程。同时对1975年至2012年间发表的有关脊柱术后脑脊液漏的英文文献进行了检索,排除有关脑脊液漏的非临床论文及OPLL术后脑脊液漏的相关论文。
结果提示,随访期内共有1223例患者接受了ACDF手术,13例患者确诊为脑脊液漏,发病率为1%。随访时间0-120个月,平均29个月。所有脑脊液漏均在术中确认,并进行一期修补术,主要方法包括:肌肉筋膜修补、生物蛋白胶、明胶海绵及胶原基质。8例患者一期修补效果满意,术后未再出现体位/姿势性头痛、颈部肿块、吞咽困难及伤口问题等脑脊液漏的相关症状。5例患者因术后存在顽固性脑脊液漏,治疗方法包括:腰大池引流、再次手术修补、脑室-腹腔分流术。随访期内所有患者症状均消失,最后完全康复。
文献回顾共检索到8篇相关论文,其中7篇为个案报道(8例),1篇为病例报道(13例),共21例脑脊液漏患者,作者根据经验提出了治疗方案。
治疗策略
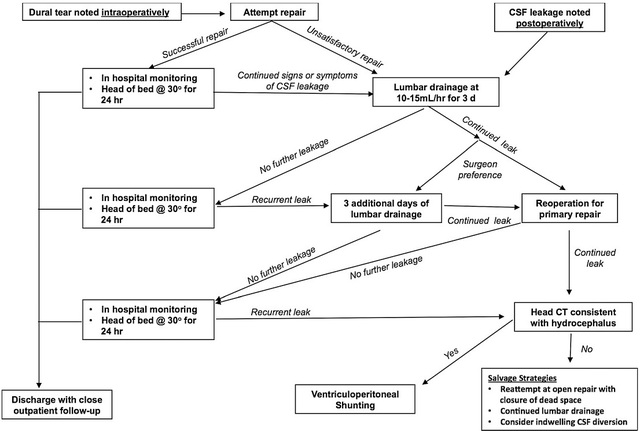
根据病例回顾及文献分析,作者提出了规范性的治疗策略(图3.)。

图3.ACDF术后脑脊液漏处理策略.
(1)首先在术中确定硬膜囊破裂,同时予以一期修补以免再次手术。从技术层面上讲,由于手术野较小,操作空间极其有限,而且紧贴脊髓,正常硬膜囊非常有限,因此一期修补难度较大,几乎无法完成修补。强行缝合有可能会加重硬膜囊缺损或使硬膜囊破口扩大。
(2)术中可采用明胶海绵、人造硬膜补片、生物蛋白胶、喷雾密封剂或上述方法结合进行修补而不是直接缝合修补,这些方法对绝大多数患者是比较有效的。
(3)可以将肌肉筋膜置于硬膜破损处,再以生物蛋白胶封闭。需要注意的是,在修补时必须确认不会对脊髓造成压迫,以免再次手术,这一点非常重要。
(4)术后患者头部抬高30°以减少对修复区域的静态压力。该体位会引起低颅压反应,从而会造成患者头痛,可以给予晶体液和咖啡因注射液对症治疗,效果通常比较满意。
(5)对于一期修复仍然不能控制脑脊液漏或者出现迟发性脑脊液漏的患者,腰大池持续引流是早期有效的治疗方法。腰大池引流管留置时间大约为3天,引流量为10-15ml/hr,通过影像学确认脑脊液没有积聚后可拔除引流管。
(6)如果脑脊液漏继续发展,接下来的步骤是再次手术,找到硬膜囊破损部位并予以修补。对于迟发性脑脊液漏、尤其是颈椎多节段手术的患者,如果不能确定硬膜囊缺损的位置,则需要行脊髓造影予以明确脑脊液漏的确切位置。采用肌肉筋膜、明胶海绵或人工硬膜覆盖和生物蛋白胶封闭的方式进行延期修补是最佳的方法。再次手术修补后需要行腰大池引流72小时。
(7)如果手术修补和腰大池引流没有效果,应当行头颅CT检查,可考虑行脑脊液持续引流,作者建议行脑室-腹腔分流术。
原始出处
Syre P1, Bohman LE, Baltuch G, Le Roux P, Welch WC.Cerebrospinal fluid leaks and their management after anterior cervical discectomy and fusion: a report of 13 cases and a review of the literature.Spine (Phila Pa 1976). 2014 Jul 15
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Spine#
29
#处理策略#
37
#融合#
28
#融合术#
30
#脑脊液漏#
34