NEJM:Semagacestat用于老年性痴呆的III期临床研究失败
2013-07-26 MedSci MedSci原创
礼来公司的治疗老年性痴呆的药物Semagacestat III期临床研究结果公布,发现Semagacestat 并不能改善老年性痴呆患者的认知功能。 Semagacestat 是特异性针对Aβ蛋白斑块,能够γ-secretase的小分子抑制剂。此次是一项双盲,安慰剂对照的试验,共纳入1537例患者,随机后治疗给予Semagacestat 治疗76周。认知功能评分ADAS-cog和ADC
礼来公司的治疗老年性痴呆的药物Semagacestat III期临床研究结果公布,发现Semagacestat 并不能改善老年性痴呆患者的认知功能。
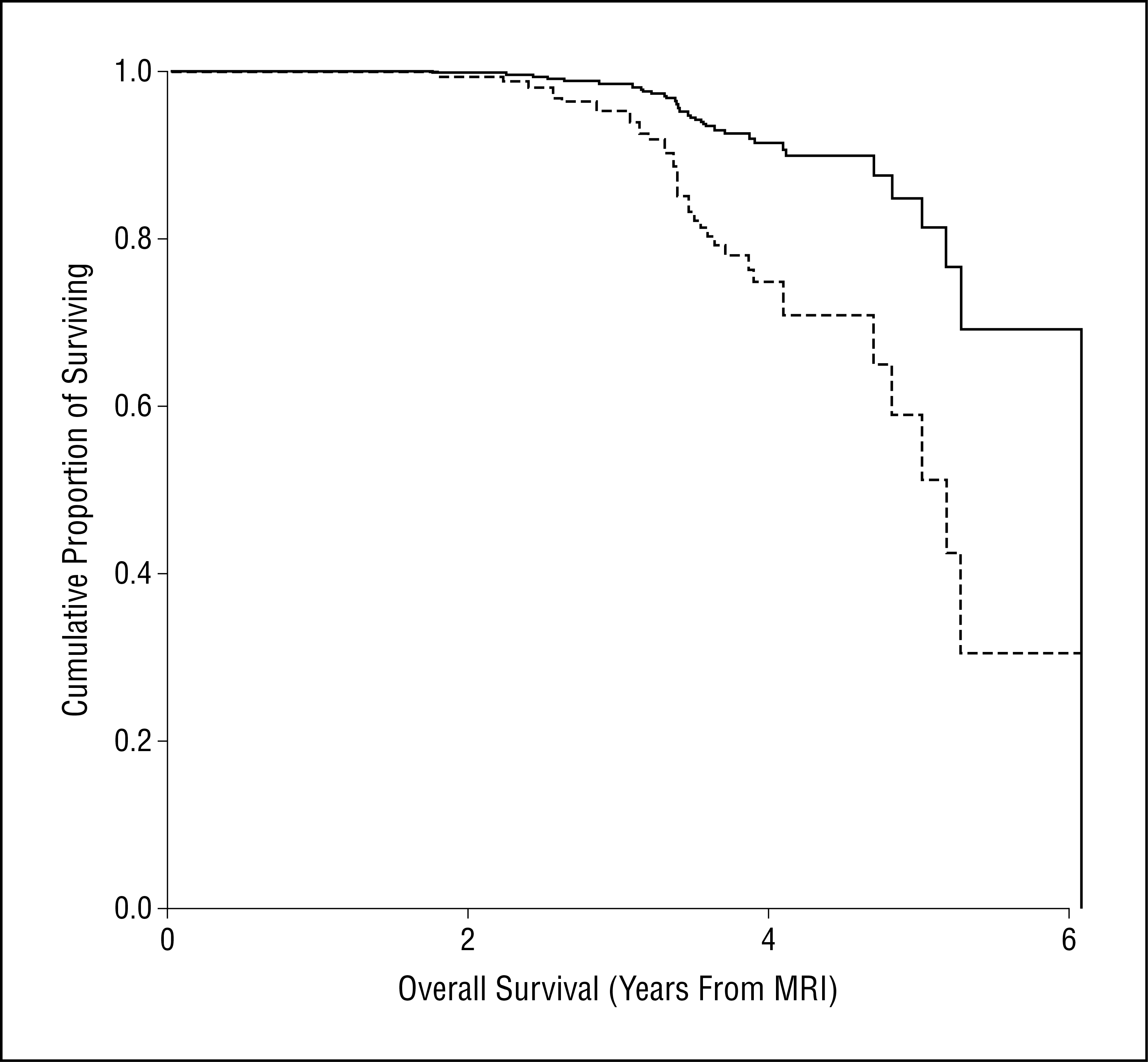
Semagacestat 是特异性针对Aβ蛋白斑块,能够γ-secretase的小分子抑制剂。此次是一项双盲,安慰剂对照的试验,共纳入1537例患者,随机后治疗给予Semagacestat 治疗76周。认知功能评分ADAS-cog和ADCS-ADL作为重要评价指标。本研究因为安全问题提前中止。入组人群中189例是安慰剂人群,153例是治疗组接受100 mg Semagacestat 治疗,121例患者接受140mg Semagacestat 治疗。三组患者ADAS-cog得分分别下降6.4, 7.5, 7.8分。ADCS-ADL评分分别下降−9.0,−10.5,−12.6 分。高剂量组与安慰剂有明显差异(P<0.001)。然而,治疗患者有明显的体重下降和更多的皮肤癌和皮肤癌风险增加,因此提前中止研究。实验室检查异常包括T淋巴细胞,免疫球蛋白,尿酸水平等变化。因此,semagacestat 并不能改善患者认知功能,高剂量甚至恶化功能。
礼来研究实验室的严伦博(Jan Lundberg)表示:“这是一次挫折,但礼来战胜阿尔兹海默症的承诺不会动摇。”。MedSci编辑也认为,虽然在老年性痴呆的治疗上探索出现了短期的挫折,但是人类攻克老年性痴呆的信心仍旧继续!
原始出处:
Doody RS, Raman R, Farlow M, Iwatsubo T, Vellas B, Joffe S, Kieburtz K, He F, Sun X, Thomas RG, Aisen PS; Alzheimer's Disease Cooperative Study Steering Committee, Siemers E, Sethuraman G, Mohs R; Semagacestat Study Group.A phase 3 trial of semagacestat for treatment of Alzheimer's disease. N Engl J Med. 2013 Jul 25;369(4):341-50.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#EST#
35
#III期临床研究#
36
#I期临床#
35
#AGA#
30
#II期临床研究#
28
#III#
23
#ACE#
33
AD防治道路任重道远
121
#EMA#
25
#II期临床#
26