Hypertension:需要警惕,高密度脂蛋白胆固醇也不是越高越好!
2022-08-23 MedSci原创 MedSci原创
该研究的数据表明高密度脂蛋白胆固醇水平与男性高血压患者心血管事件风险之间存在U型关联。
多年来,高密度脂蛋白胆固醇(HDL-C)被认为与心血管风险之间呈负相关性,这一假设主要基于流行病学研究的结果。它们表明HDL-C每增加1mg/dL,心血管死亡风险就会降低约2%至3%。然而,最新的流行病学和遗传学调查结果表明,HDL-C水平可能不能预测所有受试者的心血管预后。
最近,在无心血管疾病人群中进行的研究发现非常高的HDL-C水平可能与死亡风险增加有关。然而,HDL-C水平与特定心血管事件之间的确切关系仍然未知,尤其是在高血压患者等高危人群中。
为了进一步澄清这个问题,近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员在意大利南部Campania Salute网络中分析了高血压患者HDL-C水平与心血管事件之间的关系。
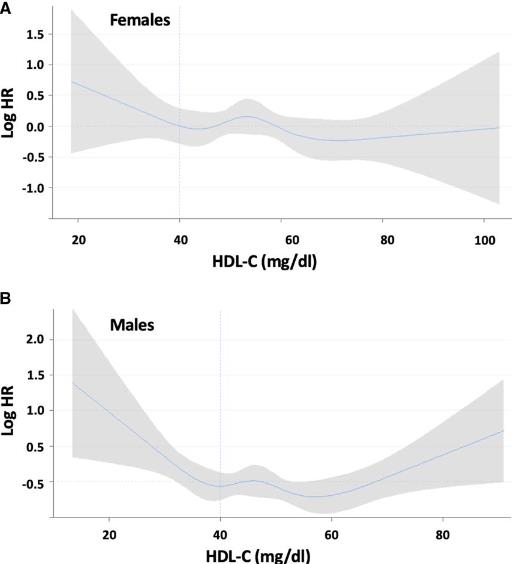
该研究的工作人员分析了11987名高血压患者,并对他们进行了25534人次每年的随访。根据血浆HDL-C水平将参与者分为3组:HDL-C<40mg/dL(低HDL-C组);HDL-C在40-80mg/dL之间(中等HDL-C组);HDL-C>80mg/dL(高HDL-C组)。在后续分析中,调整了潜在的混杂因素,研究人员观察到与中等HDL-C组相比,低HDL-C组和高HDL-C组共发生245起心血管事件,心血管事件的风险也显著升高。样条分析显示HDL-C水平与心血管预后之间存在非线性U型关联。有趣的是,与高HDL-C相关的心血管风险增加并没有在女性患者中得到证实。
由此可见,该研究的数据表明高密度脂蛋白胆固醇水平与男性高血压患者心血管事件风险之间存在U型关联。
原始出处:
Valentina Trimarco.et al.High HDL (High-Density Lipoprotein) Cholesterol Increases Cardiovascular Risk in Hypertensive Patients.Hypertension.2022.https://www.ahajournals.org/doi/epdf/10.1161/HYPERTENSIONAHA.122.19912
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TENS#
43
#PE#
35
#脂蛋白#
44
#高密度脂蛋白胆固醇#
48
#Hypertension#
53