J Clin Oncol:Poziotinib治疗既往经治的晚期或转移性NSCLC患者的疗效和安全性
2021-12-01 yd2015 MedSci原创
研究表明,Poziotinib在既往治疗过的HER2外显子20插入NSCLC患者中显示了良好的抗肿瘤活性。
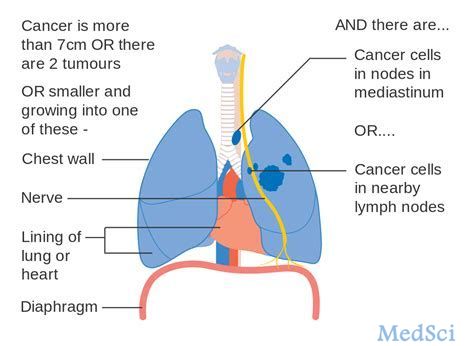
在2%-5%的非小细胞肺癌(NSCLC)患者中可以检测到HER2外显子20的插入突变,并且与不吸烟状态、女性和腺癌组织学等相关。到目前为止,还没有批准针对这一人群的靶向治疗;临床需求仍未得到满足。Poziotinib是一种不可逆的泛erbb抑制剂,具有抑制HER1突变或插入的活性(ErbB1;表皮生长因子受体[EGFR])、HER2 (ErbB2)和HER4 (ErbB4)。临床前研究提示Poziotinib对HER2外显子20的插入突变有活性。因此,国外学者开展了ZENITH20研究,旨在评估在既往经治的晚期或转移性NSCLC患者的疗效和安全性。队列2的相关结果发表在Journal of Clinical Oncology杂志上。
ZENITH20是一项多中心、多队列、开放标签的II期研究,评估poziotinib在晚期或转移性NSCLC患者中的疗效和安全性。在队列2中,患者接受poziotinib (16mg)每日一次。主要研究终点为由独立审查委员会(BICR)评估的客观缓解率(RECIST v1.1);次要观察指标为疾病控制率、应答持续时间、无进展生存期、安全性和耐受性,评估生活质量。
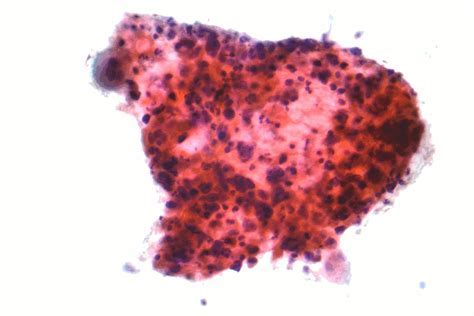
2017年10月至2021年3月,ZENITH20队列2共纳入90例患者。平均年龄为60岁,64.4%为女性,65.6%为从不吸烟者。在研究开始时,96.7%的患者有腺癌组织病理学检查,3.3%有鳞状细胞癌,15.6%有稳定的中枢神经系统转移。中断治疗的主要原因是进展性疾病(53例[58.9%])和AEs(13例[14.4%])。
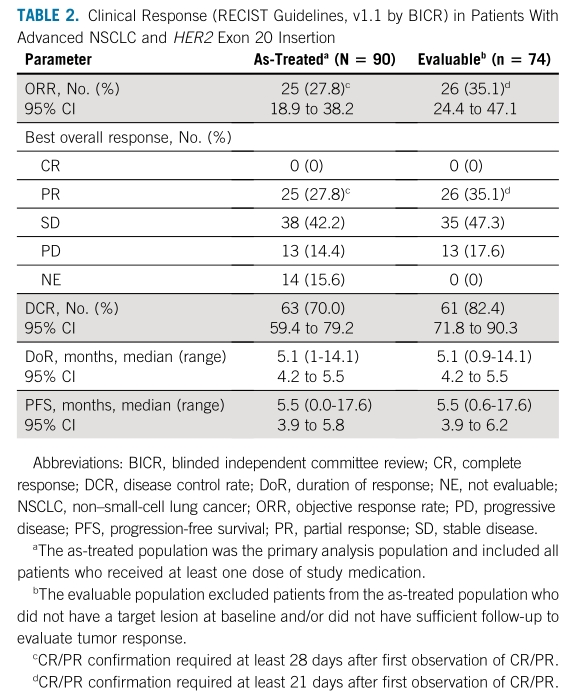
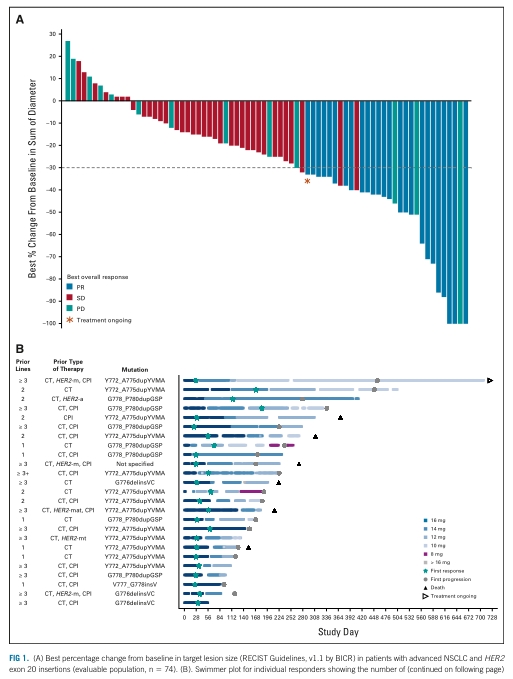
在初始分析人群中,ORR为27.8%(95%CI, 18.9 ~ 38.2), 90例接受治疗的患者中有25例达到部分缓解(PR),无患者达到完全缓解(CR)。DCR为70.0% (95% CI, 59.4 ~ 79.2)。16例患者因为各种原因排除在可评估人群外,因此可评估人群(n=74)的ORR和DCR分别为35.1% (95% CI, 24.4 - 47.1)和82.4% (95% CI, 71.8 - 90.3)。大多数患者伴有肿瘤收缩(治疗人群:74.4%[67 / 90],可评估人群:90.5%[67 / 74])。
疗效评估
在25名应答者中,中位治疗至应答时间为32天(范围:23-183天),中位DoR为5.1个月(95% CI, 4.2至5.5),24%患者DoR>6个月。所有90例接受治疗的患者的中位PFS为5.5个月(95% CI, 3.9 - 5.8), 6个月时PFS率为37.8% (95% CI, 25.5 - 50.0)。
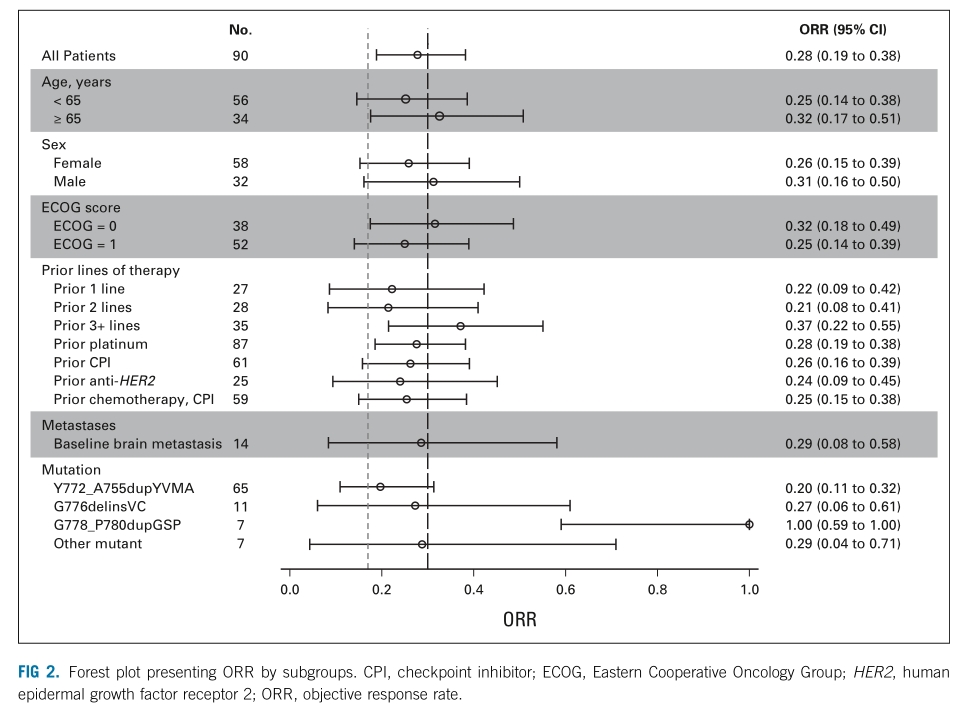
亚组分析分析,既往接受≥3线治疗患者中, ORR为37.1% (95% CI, 21.5-55.1;n=35);既往接受2线治疗患者中, ORR为21.4% (95% CI, 8.3 - 41;n =28);既往接受1线治疗患者中, ORR为22.2% (95% CI, 8.6 ~ 42.3;n=27)。
亚组分析
该队列中观察到的HER2插入突变的分布模式与之前的文献一致。HER2 Y772_A775dupYVMA突变最为频繁,在65例(72.2%)患者中发生,其ORR为20.0% (95% CI: 11.1%-31.8%),中位DoR为5.2个月,中位PFS为5.4个月。在G778_P780dupGSP或G776delinsVC突变的患者中,ORR分别为100% (n =7)和27.3% (n =11);中位PFS分别为7.6个月和3.9个月;平均DoR分别为5.3个月和4.6个月。
所有患者均发生治疗急性AEs。88例(97.8%)患者报告了治疗相关AEs (TRAEs),其中71例(78.9%)为3级,4例(4.4%)为4级。最常见的TRAE是皮疹(91.1%)、腹泻(82.2%)和口炎(68.9%);≥3级的有皮疹(48.9%)、腹泻(25.6%)和口炎(24.4%)。大多数患者(76.7%)的poziotinib剂量需要减少,中位相对剂量强度为71.5%。13.3%的患者因治疗相关不良事件而永久停止治疗。

AEs
综上,研究表明,Poziotinib在既往治疗过的HER2外显子20插入NSCLC患者中显示了良好的抗肿瘤活性。
原始出处:
Le X, Cornelissen R, Garassino M, Clarke JM, Tchekmedyian N, Goldman JW, Leu SY, Bhat G, Lebel F, Heymach JV, Socinski MA. Poziotinib in Non-Small-Cell Lung Cancer Harboring HER2 Exon 20 Insertion Mutations After Prior Therapies: ZENITH20-2 Trial. J Clin Oncol. 2021 Nov 29:JCO2101323. doi: 10.1200/JCO.21.01323. Epub ahead of print. PMID: 34843401.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Poziotinib#
0
#疗效和安全性#
31
#SCLC患者#
22
#转移性NSCLC#
35
#Oncol#
32
#转移性#
20
#NSCLC患者#
24