N Engl J Med:恩杂鲁胺有效延缓未转移前列腺癌病情进展
2018-08-06 飞奔的小马 肿瘤资讯
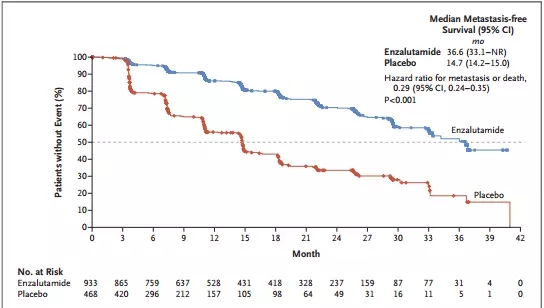
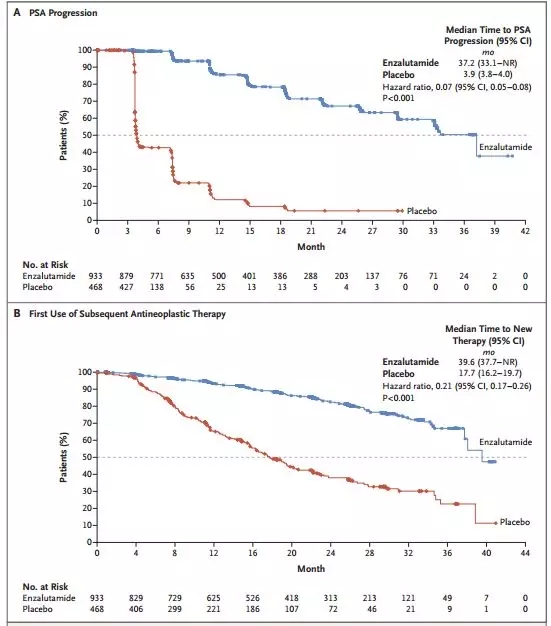
对于那些未转移的去势抵抗性前列腺癌患者来说,如果出现PSA的迅速升高,则很可能预示着患者存在较高的转移风险,前期的研究已经证实,恩杂鲁胺可以延长转移性去势抵抗性前列腺癌患者的总体生存期,那么它是否能够同样有效于未转移的去势抵抗性前列腺癌呢?其对延缓此类患者的肿瘤转移时间和PSA升高情况能否起到更多的帮助呢?近日,Maha Hussain等人报道了他们关于此方面的临床研究[1],为此类病人的化疗
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Eng#
26
#病情#
36
#Engl#
25
#Med#
32
学习了
51
了解一下谢谢
48