Hepatology:温医大团队发现肝纤维化治疗新靶点FGF12
2022-07-17 温州医科大学 温州医科大学
研究指出了FGF12是一种调控肝脏功能稳态的重要因子,同时也表明了FGF12作为肝脏纤维化损伤治疗靶点的可行性。
近日,李校堃院士团队金利泰课题组在国际肝脏病学权威期刊Hepatology在线发表研究性论文,详细介绍了肝脏纤维化病变过程中成纤维细胞生长因子12(FGF12)所扮演的角色及相关机制,并阐明巨噬细胞中的FGF12具有促进肝脏纤维化病变的功能作用,为肝脏纤维化/肝硬化的治疗提供了新的研究思路及靶点。药学院丛维涛研究员,金利泰教授,李校堃院士为论文共同通讯作者;药学院博士研究生李三铁,附属第二医院肝胆胰外科周斌主任和附属第一医院中心实验室薛梅为共同第一作者。
肝脏纤维化是各类急慢性肝病所伴随的一种严重并发症,若不进行早期干预,其往往会导致肝硬化甚至肝癌的产生,严重威胁患者的生命健康。FGF12是成纤维细胞生长因子家族中一种典型的自分泌型细胞生长因子,与常见的FGF2、FGF10或FGF21不同,FGF12不需要依赖于生长因子受体发挥下游相关作用,前期研究往往认为FGF12主要在神经元以及心肌细胞中表达,具有调控离子通道以及心肌节律的关键作用,但FGF12在肝脏稳态调控以及肝脏纤维化病变过程中的作用和机制目前尚不明确。
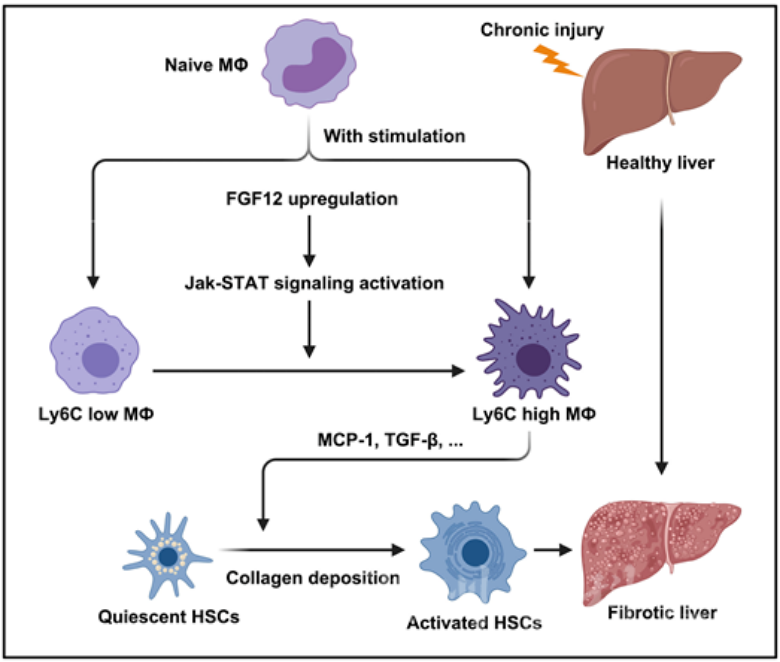
课题组的研究表明,FGF12的表达水平在不同的肝脏纤维化模型小鼠中显著上调,且相比于肝细胞,FGF12主要表达于肝非实质细胞中,进一步的研究则证实纤维化过程中肝脏巨噬细胞可能是FGF12的主要表达来源,同时在巨噬细胞特异性FGF12敲除小鼠中,课题组发现胆管结扎以及四氯化碳注射所诱发的肝脏纤维化得到了明显的缓解,表明巨噬细胞中的FGF12具有促进肝脏纤维化的作用。课题组的研究同时也指出了FGF12能够上调纤维化肝脏组织中Ly6C高表达巨噬细胞的数量,并通过MCP-1/CCR2这一信号通路促进肝星状细胞的激活,从而加剧肝脏纤维化。为进一步证实FGF12与肝纤维化之间的关联,课题组在相关人体肝脏组织样本中进行了实验分析,并发现FGF12的表达与肝脏纤维化的程度呈正相关,进一步说明了FGF12调控肝纤维化发生发展的功能及作用。课题组的研究指出了FGF12是一种调控肝脏功能稳态的重要因子,同时也表明了FGF12作为肝脏纤维化损伤治疗靶点的可行性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#FGF1#
38
#肝纤维#
44
#新靶点#
40
#EPA#
44
#治疗新靶点#
52