Lancet:未破裂的脑动静脉畸形仅药物治疗就足够了吗?(ARUBA试验)
2014-02-18 何Jason 医学专业新闻
背景:未破裂脑动静脉畸形进行预防性根治的临床获益仍存在争议。ARUBA是一项随机试验,旨在比较这些患者接受单一药物治疗或药物联合介入治疗,对死亡和症状性脑卒中风险的影响。 方法:在九个国家共39个临床中心招募的未破裂脑动静脉畸形成年患者(18岁以上),被随机分配至药物联合介入治疗组(介入治疗包括神经外科手术、血管栓塞术或立体定向放射治疗,可单用或联用)、药物治疗组(如果有需要,则针对神经
背景:未破裂脑动静脉畸形进行预防性根治的临床获益仍存在争议。ARUBA是一项随机试验,旨在比较这些患者接受单一药物治疗或药物联合介入治疗,对死亡和症状性脑卒中风险的影响。【原文下载】
方法:在九个国家共39个临床中心招募的未破裂脑动静脉畸形成年患者(18岁以上),被随机分配至药物联合介入治疗组(介入治疗包括神经外科手术、血管栓塞术或立体定向放射治疗,可单用或联用)、药物治疗组(如果有需要,则针对神经症状给予药物)。患者、临床医师和研究者均清楚治疗分组。主要研究结局为出现死亡或症状性脑卒中复合终点的时间;主要分析方法为意向治疗分析。
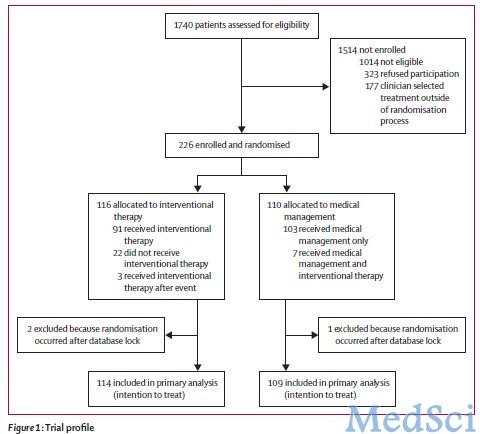
结果:2007年4月4日起启动随机分组;在2013年4月15日,在美国NIH下属国家神经疾病和卒中研究委任的数据安全监督委员会的建议下,由于药物治疗存在明显的优势,本实验的随机分组被停止。此时共有223名患者获得转归数据(平均随访33.3个月),其中介入治疗有114人,药物治疗组则由109人。在达到主要研究结局方面,药物治疗组共有11人(10.1%),而介入治疗组则有35人(30.7%)。单一药物治疗组的死亡或卒中风险明显低于介入治疗组(比值比0.27)。除了介入治疗组患者中发生卒中(45 vs 12)、及与卒中无关的神经功能损害(14 vs 1)者的数量多于药物治疗组之外,未发现其他危害。

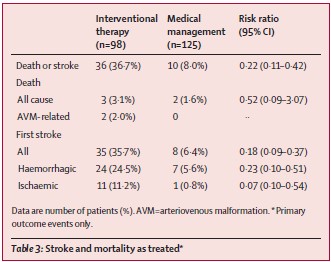
ARUBA试验表明,在 33 个月的随访期间,单一药物治疗在预防未破裂脑动静脉畸形患者死亡或中风的效果方面,优于药物联合介入治疗。 该试验仍处于观察阶段,以确定在额外5年的随访中,该差异是否持续。
原始出处:
Mohr JP1, Parides MK2, Stapf C3, Moquete E2, Moy CS4, Overbey JR2, Al-Shahi Salman R5, Vicaut E6, Young WL7, Houdart E8, Cordonnier C9, Stefani MA10, Hartmann A11, von Kummer R12, Biondi A13, Berkefeld J14, Klijn CJ15, Harkness K16, Libman R17, Barreau X18, Moskowitz AJ2; international ARUBA investigators.Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial.Lancet. 2014 Feb 15;383(9917):614-21. doi: 10.1016/S0140-6736(13)62302-8. 【原文下载】
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
40
#动静脉畸形#
40
#静脉#
43
#畸形#
39