Neurology:伴沟底发育不良的癫痫双侧结构网络异常
2021-10-29 Naomii MedSci原创
研究证明了双边分布的、特定的白质网络在BOSD中易受干扰的证据。纤维束异常的程度部分与癫痫发作活动有关,但其他因素,如遗传背景和治疗或环境的影响并未被排除在外。
目前,局灶性癫痫被广泛认为是一种网络障碍;据此,局灶性病变可以导致脑部网络的广泛异常。这些癫痫的网络概念化主要是由颞叶癫痫的证据驱动的;然而,最近的研究表明,局灶性皮质发育不良(FCD)的特征也可能是广泛的功能网络异常。目前尚不清楚FCD中是否有特定的结构网络容易受到破坏,探索全网络破坏的努力在一定程度上受到了阻碍。
沟底发育不良(BOSD)是一种FCD,具有独特的神经病理和神经影像学特征。考虑到手术后的良好结果,BOSD病变被认为是固有的癫痫样病变,被认为是局灶性异常,而不是弥漫性病变。然而,与其他形式的局灶性癫痫一样,BOSD可能与更广泛的脑组织破坏有关。然而,目前尚不清楚BOSD是否以特定大脑网络中断为特征,如果是的话,哪些结构网络受到影响。
近日,有研究人员应用了一种被称为基于固定的分析(FBA)的技术,该技术能够识别特定的白质结构,这些白质结构表现出临床上重要的结构连通性降低,从而鉴定脑沟底发育不良(BOSD)患者脑白质纤维束的结构异常,并探讨其与癫痫发作活动的关系。
对弥散磁共振成像数据进行了基于全脑固定的分析,以确定与健康对照组参与者(n=40)相比,BOSD患者(n=20)的白质纤维束的纤维密度和横截面显著降低。以全脑分析结果为先验,探讨纤维束异常与癫痫发作频率和持续时间的关系。
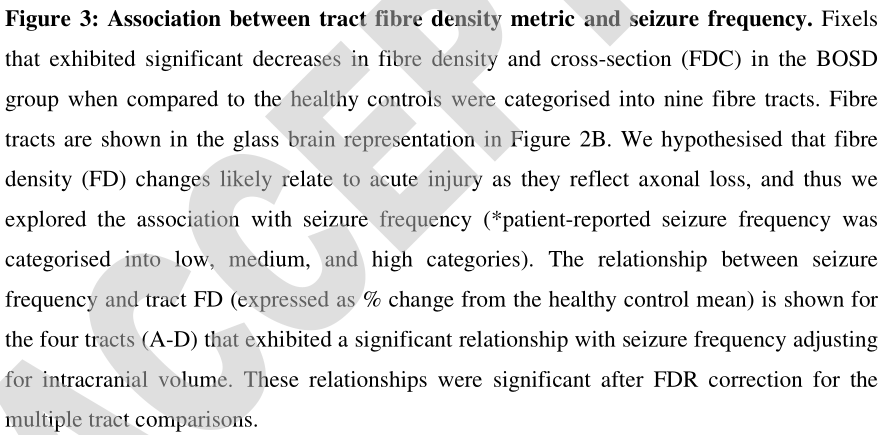
- 尽管异常增生是局灶性的,但BOSD患者表现出广泛的白质纤维束异常,包括双侧皮质脊髓、皮质丘脑和小丘脑束、上纵束、胼胝体(体)和胼胝体辐射线枕部。这种双侧连通性降低的模式与病变的偏侧性无关。
- 事后探索性分析显示,高癫痫发作频率与钳子主束、双侧皮质脊髓束和小丘脑束纤维密度降低程度更大相关。
研究证明了双边分布的、特定的白质网络在BOSD中易受干扰的证据。纤维束异常的程度部分与癫痫发作活动有关,但其他因素,如遗传背景和治疗或环境的影响并未被排除在外。
文献来源:Mito R, Vaughan DN, Semmelroch M, Connelly A, Jackson GD. Bilateral Structural Network Abnormalities in Epilepsy Associated With Bottom-of-Sulcus Dysplasia [published online ahead of print, 2021 Oct 21]. Neurology. 2021;10.1212/WNL.0000000000013006. doi:10.1212/WNL.0000000000013006
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Neurol#
36
#发育#
38
#双侧#
37
#发育不良#
54