BJU Int:术中冷冻切片鉴定根治性前列腺切除术后存在BCR风险的患者
2021-05-24 AlexYang MedSci原创
前列腺癌(PCa)患者在根治性前列腺切除术(RP)后的阳性手术边缘与不利的肿瘤学结果有关。为了降低手术边缘阳性率并同时保留神经血管束,可以在RP期间进行术中全包埋冷冻切片(FS)。根据术中冷冻切片的结
前列腺癌(PCa)患者在根治性前列腺切除术(RP)后的阳性手术边缘与不利的肿瘤学结果有关。为了降低手术边缘阳性率并同时保留神经血管束,可以在RP期间进行术中全包埋冷冻切片(FS)。根据术中冷冻切片的结果,可以在RP期间进行二次肿瘤切除。这种方法可以减少最终手术边缘呈阳性的患者数量,同时可以允许采用个性化的、肿瘤学上合理的方法来保留神经血管束。

近期,有研究人员鉴定了前列腺癌根治术后有生化复发风险的患者,并在术中对前列腺进行全包埋冷冻切片。他们调查了FS中最初手术边缘阴性的患者、FS中最初手术边缘阳性但二次肿瘤切除后没有残留PCa的患者、以及FS中最初手术边缘阳性且二次肿瘤切除标本中有残留PCa的最终手术边缘阴性的患者之间的BCR差异。

研究人员共收集了883名接受RP治疗的连续患者的机构数据。术中采用全包埋FS检查边缘状态,且必要时切除更多的前列腺周围组织以达到阴性边缘。分析中排除了淋巴结阳性的患者或最终手术边缘阳性的患者。
结果发现,随访的中位数为22.4个月。与初始R0状态的患者(93.4%,90.9%)相比,进行二次肿瘤切除后有残余PCa的患者(81.0%,72.9%,p=0.001)和无残余PCa的患者(90.3%,82.3%,p=0.033)的1年和2年BRFS率显著更低。在多变量Cox回归中,与初始R0状态相比,只有二次肿瘤切除后的残留PCa与BCR更高的风险有关(HR 1.99, 95%CI 1.01-3.92, p=0.046)。
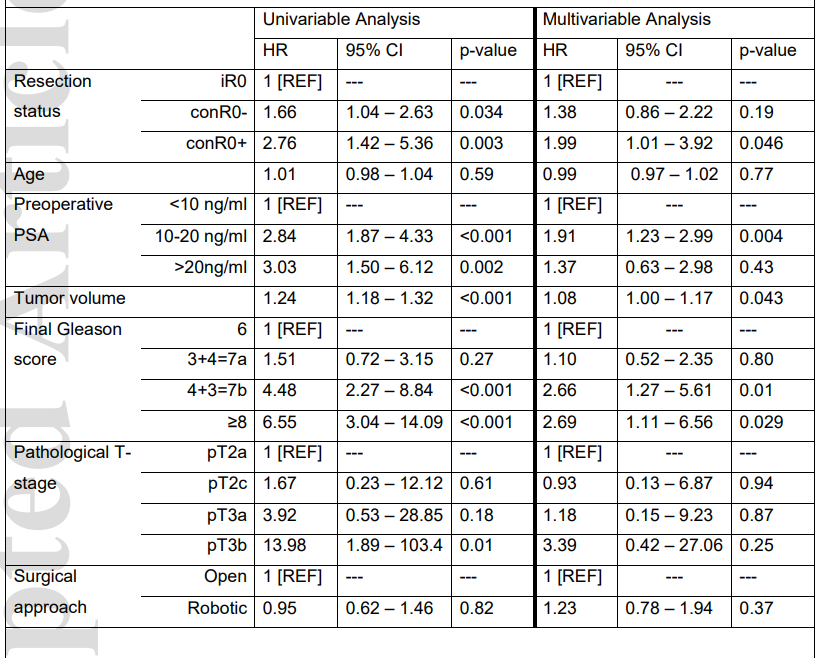
单变量和多变量Cox比例风险回归调查根治性前列腺切除术后的生化复发风险情况
尽管被归类为阴性手术边缘,但二次肿瘤切除标本中有残留PCa的患者仍旧面临高风险的BCR。他们的发现强调了对这一特定亚组应进行更密切的术后监测。进一步的研究应着重于研究这些患者是否能从早期挽救治疗中获益,以及在不断变化的PCa治疗中,切除状态如何影响肿瘤学结果。
原始出处:
Karl H Tully , Max Schulmeyer , Julian Hanske et al. Identification of patients at risk for BCR after radical prostatectomy with intraoperative frozen section. BJU Int. May 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#切除术#
36
#冷冻切片#
0
#前列腺切除#
51
认真学习
0
#根治#
36
认真学习
60