Movement Disorder : 胶质细胞成像,可鉴别帕金森和多系统萎缩
2021-10-30 Freeman MedSci原创
MSA患者的区域神经胶质TSPO结合明显增加的模式。
多系统萎缩(MSA)是一种罕见的致命的神经系统疾病,病因不明。其临床表现的特点是运动和自主神经功能障碍。根据运动表现,MSA被分为帕金森型(MSA-P)和小脑型(MSA-C)。
 一个主要的临床挑战是如何区分MSA-P和PD或MSA-C和特发性晚发性小脑共济失调之间的关系。尽管目前的临床诊断标准在疾病后期表现良好,但据报道,首次检查的敏感性仅达到30%左右,而且明确的MSA诊断仍依赖于死后检查。因此,开发敏感的生物标志物用于早期诊断是一个重要的医学需求,特别是在疾病改造试验的病人招募方面。
一个主要的临床挑战是如何区分MSA-P和PD或MSA-C和特发性晚发性小脑共济失调之间的关系。尽管目前的临床诊断标准在疾病后期表现良好,但据报道,首次检查的敏感性仅达到30%左右,而且明确的MSA诊断仍依赖于死后检查。因此,开发敏感的生物标志物用于早期诊断是一个重要的医学需求,特别是在疾病改造试验的病人招募方面。
MSA的神经病理学特点是胶质和神经元的细胞质内含物,其中含有折叠错误的α-突触核蛋白(αSYN),特别是导致黑质和小脑结构中神经元的突出损失。MSA的病理进展伴随着神经炎症,表现为促炎症细胞因子水平的升高和广泛的小胶质增生。 一小部分MSA患者体内的胶质反应已被报道,使用正电子发射断层扫描(PET)成像的易位蛋白(TSPO)是小胶质细胞和星形细胞的标志物。因此,TSPO成像可以提供关于MSA病理生理学的额外信息,并有可能用于诊断目的。
藉此,卡洛琳斯卡大学的Aurelija Jucaite等人,研究了TSPO成像对MSA和PD以及MSA亚型之间的诊断敏感性和特异性。除了视觉阅读,他们还应用了机器学习(ML)方法来获得MSA的胶质细胞成像特征。
他们利用66名MSA患者和24名PD患者的影像资料分析了[11 C]PBR28与TSPO的结合。组别比较是基于参数图像的区域分析。诊断读数包括针对临床诊断和机器学习分析的PET图像的视觉读数。敏感性、特异性和ROC曲线被用来区分MSA和PD以及小脑和帕金森变异MSA。
他们发现:与PD相比,MSA的区域性[11 C]PBR28与TSPO的结合明显升高,"热点 "出现在天形核和小脑白质。
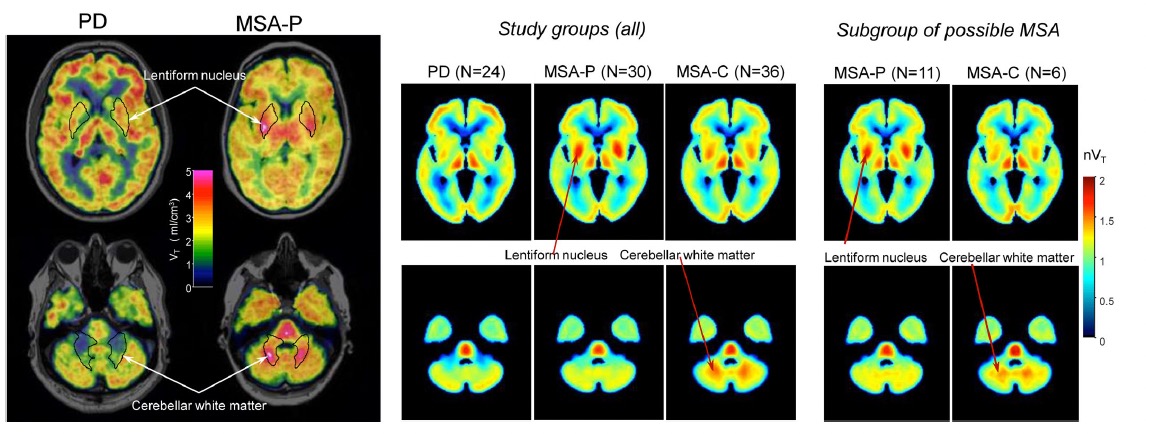
视觉阅读将MSA与PD区分开来,特异性为100%,敏感性为83%。机器学习方法将敏感性提高到96%。并确定了MSA亚型特异的TSPO结合模式。
该研究的主要意义在于发现了:MSA患者的区域神经胶质TSPO结合明显增加的模式。有趣的是,其数据与MSA的严重神经炎症相一致。神经胶质成像可能有潜力支持临床MSA的诊断和病人分层,以进行新的药物治疗的临床试验。
原文出处:
Jucaite A, Cselényi Z, Kreisl WC, et al. Glia Imaging Differentiates Multiple System Atrophy from Parkinson’s Disease: A Positron Emission Tomography Study with 11C PBR28 and Machine Learning Analysis. Mov Disord. Published online October 5, 2021:mds.28814. doi:10.1002/mds.28814
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





















#Disord#
40
#萎缩#
34
#disorder#
26
#Dis#
25
#胶质细胞#
40
#多系统萎缩#
41
学习
67