BMJ:溶栓治疗并发自发性舌血肿——案例报道
2016-11-17 MedSci MedSci原创
患者男,71岁,静脉阿替普酶和肝素治疗后3小时后,出现言语和吞咽困难。 患者因为肺栓塞引起血流动力学不稳定,所以使用这两种药物治疗,阿替普酶的治疗剂量为10 mg静脉推注,然后90 mg静脉滴注(超过两小时)。 查体发现舌严重肿胀和瘀斑,提示舌血肿。除抗凝/溶栓治疗外,没有发现其他病因。 对患者的气道进行密切监测,最终没有进行干预,患者就自行恢复了。 溶栓治疗过程中
患者男,71岁,静脉阿替普酶和肝素治疗后3小时后,出现言语和吞咽困难。
患者因为肺栓塞引起血流动力学不稳定,所以使用这两种药物治疗,阿替普酶的治疗剂量为10 mg静脉推注,然后90 mg静脉滴注(超过两小时)。
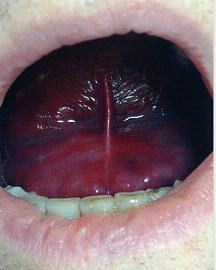
查体发现舌严重肿胀和瘀斑,提示舌血肿。除抗凝/溶栓治疗外,没有发现其他病因。
对患者的气道进行密切监测,最终没有进行干预,患者就自行恢复了。
溶栓治疗过程中大约有5%的患者会出现出血或血肿形成并发症。出血性事件通常限于注射部位,不过临床医生应该意识到,自发性出血还可以发生在其他与注射部位不相关的部位,此外还应注意轻微外伤后的出血风险。
原始出处:
Alexander Bobinskas,et al.Spontaneous lingual haematoma secondary to thrombolysis.BMJ 2016;355:i5569
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#BMJ#
27
#并发#
33
#血肿#
39
#溶栓治疗#
37
#自发性#
41