退变性滑脱椎管狭窄:微创减压融合vs传统PLIF
2012-08-20 zhanghaisen 丁香园
随着微创理念在骨科领域的不断深入,退变性脊柱疾病的微创手术治疗,临床报道不断增多。传统意义上,退变性椎体滑脱所致的腰椎管狭窄症可采用后路椎管减压椎体间融合(posterior lumbar interbody fusion, PLIF)手术治疗,但这类疾病采用微创经皮椎管减压后外侧融合手术(MIS-PLF)治疗较之传统开放手术的效果如何,尚无临床报道。&nbs
随着微创理念在骨科领域的不断深入,退变性脊柱疾病的微创手术治疗,临床报道不断增多。传统意义上,退变性椎体滑脱所致的腰椎管狭窄症可采用后路椎管减压椎体间融合(posterior lumbar interbody fusion, PLIF)手术治疗,但这类疾病采用微创经皮椎管减压后外侧融合手术(MIS-PLF)治疗较之传统开放手术的效果如何,尚无临床报道。
近日,日本东京大学医学院脊柱重建外科的Yoshihisa等实施了一项临床对比研究,对传统PLIF与MIS-PLF治疗退变滑脱性椎管狭窄的临床效果进行了比较,相关研究结果发表于近期出版的Eur Spine J杂志。
该研究共涉及采用单节段PLIF手术治疗的80例退变滑脱性腰椎管狭窄症患者,其中43例接受MIS-PLF,另外37例接受开放性PLIF。MIS-PLF手术的皮肤切口约为4cm,采用专用器械经皮置入椎弓根螺钉,之后微创下神经减压,最后实施横突内侧髂骨植骨。开放性PLIF采用传统常规方法实施。术后至少随访2年。评价指标包括手术时间,术中、术后失血量,Oswestry功能障碍指数(ODI),Roland-Morris调查表(RMQ),日本骨科学会评分以及视觉模拟腰痛量表等。另外,还对手术的融合率及并发症发生率进行考察。
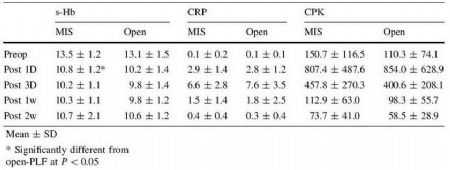
表1.两组病例的术前数据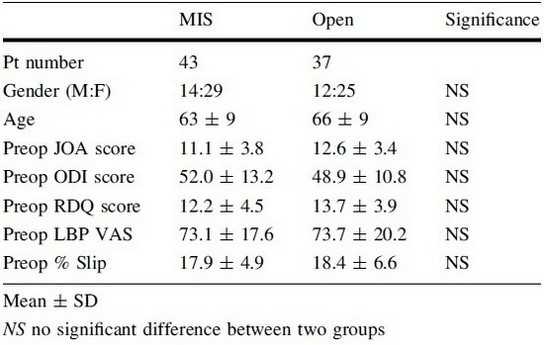

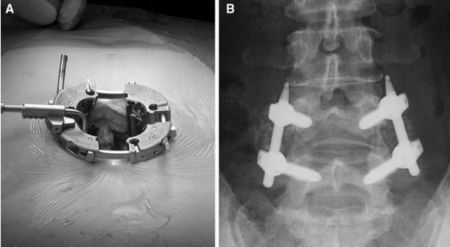
图1.经皮置入Sextant 脊柱微创操作系统器械(Medtronic, Memphis, TN, USA)
数据结果显示,两组的手术时间差异无统计学意义,MIS-PLF组(181 ml)的术中失血量显着低于开放PLIF组(453 ml)。术后第1天的失血量MIS-PLF组(210 ml)也较之开放PLIF组为低(406 ml)。MIS-PLF组的ODI与RMQ评分在术后最初2周迅速降低,并在术后3, 6, 12及24个月一直低于开放PLIF组水平。两组的融合率差异无统计学意义(98 vs. 100%),均无重大并发症发生。
最后,作者指出,经皮椎弓根固定MIS-PLF较之传统开放式PLIF手术更为微创,术后疼痛水平的降低会有助于患者日常行为活动的提高,进而使多项功能评分水平得以改善。MIS-PLF组的优势水平可持续维持到术后2年,这表明在减轻腰痛,改善患者日常行为功能方面,微创PLF手术的中期效果更佳。除了传统开放式PLIF手术,MIS-PLF是治疗退变滑脱性腰椎管狭窄症的另一有效术式。
表2.两组的实验室检查数据对比
图2.a、经皮置入扩大牵开器,扩大术野,以便于MIS-PLF手术操作。b、后外侧玻璃横突内侧皮质之后,实施双侧髂骨颗粒植骨。
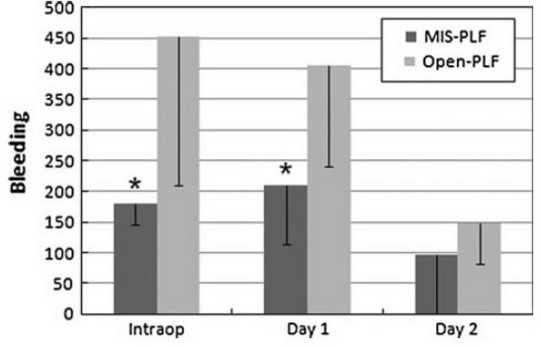
图3.两组的术中及术后1、2天失血量对比。

图4.两组不同时间点的ODI评分对比。
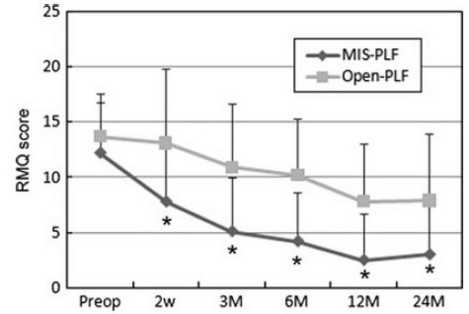
图5.两组不同时间点的RMQ评分对比。
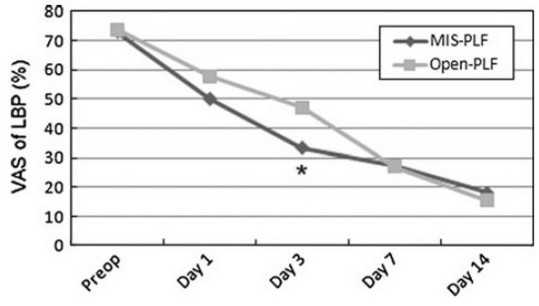
图6.两组不同时间点的视觉模拟疼痛评分对比。
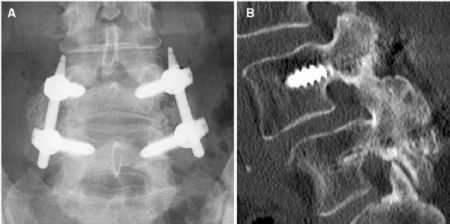
图7.MIS-PLF 1例术后29个月X线片及矢状位CT评估图像。a、正位X线片所示,后外侧连续性坚强融合;b、矢状位CT图像所示,连续性坚强融合
原文链接:
Kotani Y, Abumi K, Ito M, Sudo H, Abe Y, Minami A. Mid-term clinical results of minimally invasive decompression and posterolateral fusion with percutaneous pedicle screws versus conventional approach for degenerative spondylolisthesis with spinal stenosis. Eur Spine J. 2012 Jun;21(6):1171-7. Epub 2011 Dec 16.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#椎管#
33
#椎管狭窄#
37
#微创#
43
#变性#
39
#融合#
33