European Radiology:这些征象提示了什么?胸腺瘤、胸腺癌和淋巴瘤的影像学鉴别
2022-01-20 shaosai MedSci原创
胸腺肿瘤是前纵隔最常见的原发性肿瘤,主要包括胸腺瘤、胸腺癌、胸腺淋巴瘤和生殖细胞瘤(GCTs)。
胸腺肿瘤是前纵隔最常见的原发性肿瘤,主要包括胸腺瘤、胸腺癌、胸腺淋巴瘤和生殖细胞瘤(GCTs)。每种肿瘤类型都有不同的最佳治疗方案和预后。对于胸腺上皮性肿瘤,手术是主要的治疗手段。然而,原发性胸腺淋巴瘤一般采用放疗和化疗的方法。相比之下,恶性GCTs患者的治疗方法则不同,包括顺铂化疗在内的多模式治疗联合手术切除是首选的治疗策略。因此,在治疗前准确区分胸腺肿块以指导治疗决策至关重要。
CT和MRI是做常用的影像学检查手段,为这些病变的检测、分化、分期和预后评估提供了宝贵的诊断信息。与CT相比,MRI具有更高的软组织分辨率,尤其是T2加权成像(T2WI)可以显示肿瘤的异质性及其肿瘤内的胶原纤维成分。
近日,发表在European Radiology杂志的一项研究探讨了基于T2和弥散加权MRI的胸腺瘤、胸腺癌和淋巴瘤之间的胶原纤维模式(CFPs)差异,并评估了其在胸腺肿瘤鉴别诊断中的价值和可重复性,为术前无创诊断及鉴别提供了新的思路和参考。
回顾性地纳入了38名经病理诊断的胸腺瘤、胸腺癌和淋巴瘤患者,均接受了T2和扩散加权MR扫描。CFPs被分为四类:隔膜征、斑块状模式、混合模式和无隔膜征。比较了不同胸腺肿瘤中CFPs的发生率,并分析了区分所定义的肿瘤类型的有效性和可重复性。
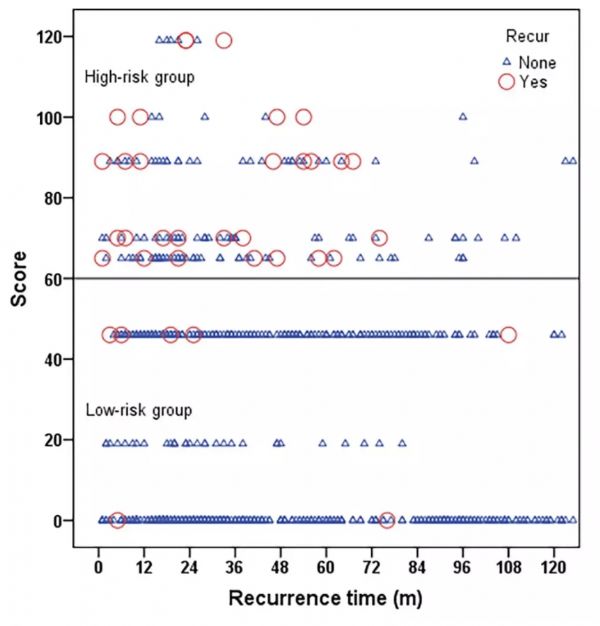
胸腺瘤、胸腺鳞状细胞癌(TSCCs)、其他胸腺癌和神经内分泌肿瘤(OTC&NTs)以及胸腺淋巴瘤之间的CFPs存在显著差异。在209个(86%)胸腺瘤中发现了隔膜征,这在胸腺瘤和任何其他胸腺肿瘤之间是不同的(所有P < 0.005)。斑块状、混合状和无隔膜征象主要分别见于TSCCs(80.3%)、OTC&NTs(78.9%)和胸腺淋巴瘤(56.9%)。两位读者对不同CFP评价的一致性为良好或优秀。CFP在识别胸腺肿瘤方面取得了很高的诊断效能。
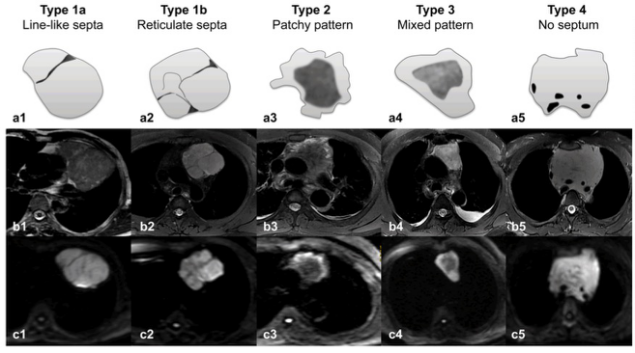
图 胸腺肿瘤的瘤内胶原纤维模式(CFP)示意图。a1-5,示意图;b1-5,T2加权图像;c1-5,弥散加权图像(b=1000s/mm2)。根据MR T2和弥散加权图像的发现,CFPs分为4种类型:1型,隔膜征,包括1a型(a1-c1,线状隔膜)和1b型(a2-c2,网状隔膜);2型,斑块状(a3-c3);3型,混合型(a4-c4);4型,无隔膜型(a5-c5)。
本研究表明,基于T2和DW MRI的CFPs有助于胸腺瘤、TSCCs和胸腺淋巴瘤的鉴别,且具有很高的效能和可重复性。因此,CFPs可以作为识别胸腺肿瘤的可靠的影像学标志物,并可增强放射科医生对胸腺肿瘤鉴别诊断的信心。
原文出处:
Yu-Chuan Hu,Wei-Qiang Yan,Lin-Feng Yan,et al.Differentiating thymoma, thymic carcinoma and lymphoma based on collagen fibre patterns with T2- and diffusion-weighted magnetic resonance imaging.DOI:10.1007/s00330-021-08143-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#胸腺癌#
30
#PE#
26
#胸腺#
35
#胸腺瘤#
34