Investigative Radiology:这一模型,实现了超声和MRI弹性成像的标准化应用!
2022-09-06 shaosai MedSci原创
临床上,不同的临床弹性成像设备在同一志愿者身上显示出不同的剪切波速度(SWS)值,这是标准化和建立定量肝脏硬度标志物的主要障碍。
 多项研究表明,组织硬度的测量是各种疾病的准确诊断标志,其中肝脏硬度可通过弹性成像和标准化参考方法(如剪切波速度)在体内进行量化。然而,目前还没有普遍接受的用于检测肝纤维化的独立于系统的肝脏硬度阈值。临床上,不同的临床弹性成像设备在同一志愿者身上显示出不同的剪切波速度(SWS)值,这是标准化和建立定量肝脏硬度标志物的主要障碍。最近,QIBA在标准化模型中比较了不同的临床弹性成像方法,得出的结论是所有的方法都能正确区分软性和硬性模型,但在有粘度的情况下设备间的偏差就会增加。
多项研究表明,组织硬度的测量是各种疾病的准确诊断标志,其中肝脏硬度可通过弹性成像和标准化参考方法(如剪切波速度)在体内进行量化。然而,目前还没有普遍接受的用于检测肝纤维化的独立于系统的肝脏硬度阈值。临床上,不同的临床弹性成像设备在同一志愿者身上显示出不同的剪切波速度(SWS)值,这是标准化和建立定量肝脏硬度标志物的主要障碍。最近,QIBA在标准化模型中比较了不同的临床弹性成像方法,得出的结论是所有的方法都能正确区分软性和硬性模型,但在有粘度的情况下设备间的偏差就会增加。
粘度引起的肝脏硬度的变化是通过SWS的分散性来测量的SWS随波频率的增加而增加。因此,只有在精确知道激励频率或用相同的激励方法进行测量时,才能在不同的模式之间比较SWS。瞬态波对应于一个更广泛的剪切波频率谱,其中中心频率通常被认为是群频。更具挑战性的是,由于粘性阻尼的作用,这个群组频率随着时间的推移而降低。因此,临床上迫切需要建立一个具有现实和精确已知的SWS分散特性的模型来描述弹性成像设备的群频率。
一些主要的弹性模型已被提议用于超声弹性成像(USE)和磁共振弹性成像(MRE),然而据我们所知,没有一个模型是专门针对肝脏的粘弹性分散和超声/MRI参数的。
近日,发表在Investigative Radiology杂志的一项研究通过使用一个全面的模拟人体肝脏SWS分散并可重复生成的特征模型,促进临床弹性成像在不同设备和平台的标准化。
本研究涉及的模型由线性聚合聚丙烯酰胺(PAAm)制成,根据文献报道的健康人体内的粘弹性能进行校准。使用拟合于PAAm剪切波速度分散的2参数弹簧壶模型来分析硬度分散,通过剪切流变仪、基于超声的时间谐波弹性成像、临床磁共振弹性成像(MRE)和频率范围为5至3000赫兹的台式MRE来测量硬度分散。评估了超声和磁共振成像的成像参数、可重复性和温度依赖性。此外,也对临床弹性成像方法(Aplio i900,佳能;Acuson Sequoia,西门子;FibroScan,EchoSense)的剪切波速度的频率带进行了描述。
在本研究分析的整个频率范围内,PAAm模型很好地再现了人体肝脏在体内的硬散布,尽管其在静态负载下具有流体特性(springpot硬度参数,2.14 [95%置信区间,2.08-2.19] kPa;springpot powerlaw指数,0.367 [95%置信区间,0.362-0.373] )。成像参数与体内肝脏的参数接近,在批次之间、6个月期间以及温度每升高一摄氏度,硬度值仅有0.5%(0.4%,0.6%)、4.1%(3.9%,4.5%)和-0.63%(-0.67%,-0.58%)的轻微变化。
 图
图
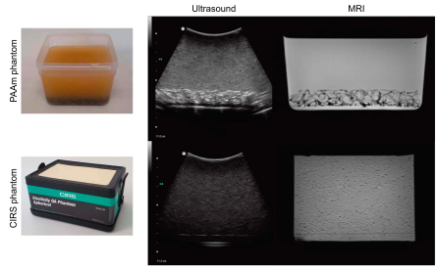
PAAm模型的成像特性。聚丙烯酰胺(PAAm)模型和CIRS模型的成像特性与超声和磁共振成像(MRI)的比较(按比例;血管的高度[CIRS,PAAm],10厘米)
本研究介绍了一个针对健康人类肝脏刚度分散的全面特征的液体肝脏模型。该模型非常适用于超声和MRI的弹性成像,因此促进了不同系统之间肝脏硬度测量的标准化。
原文出处:
Anna S Morr,Helge Herthum,Felix Schrank,et al.Liquid-Liver Phantom: Mimicking the Viscoelastic Dispersion of Human Liver for Ultrasound- and MRI-Based Elastography.DOI:10.1097/RLI.0000000000000862
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#弹性成像#
39
#标准化#
35
#EST#
31
#IgA#
35