Frontiers in Immunology:半乳糖凝集素9通过调节Treg/Th17比值调节尿酸钠晶体诱导的痛风性炎症
2021-11-12 彼岸河边草 MedSci原创
阐述半乳糖凝集素9在痛风性关节炎的发生和发展过程中调节炎症反应的具体细胞和分子机制.
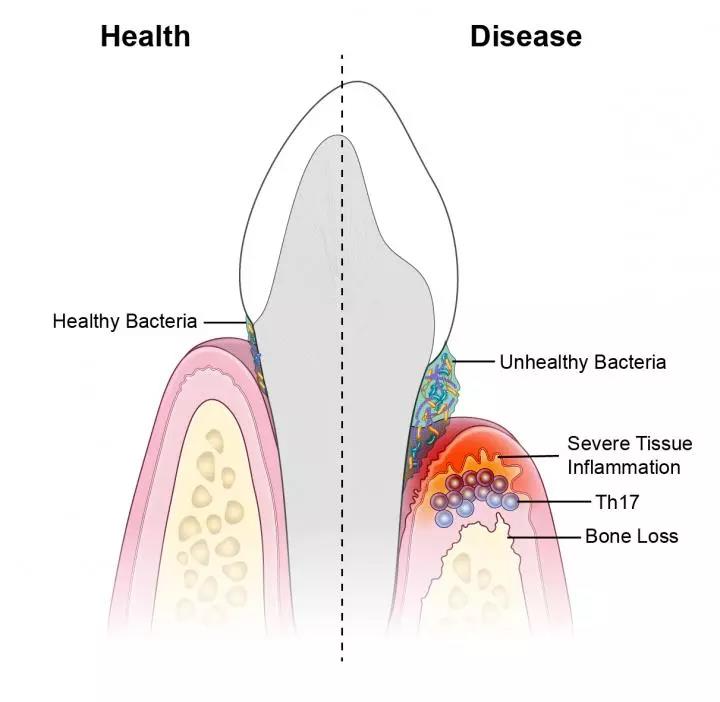
痛风是由在关节区域内沉积尿酸钠(MSU)晶体引起的。嗜中性粒细胞和单核细胞浸润驱动最初的炎症反应,然后是淋巴细胞。有趣的是,新出现的证据支持T辅助17细胞 (Th17)/调节性T细胞(Treg)的原位失衡会影响随后对靶组织的损伤的观点。半乳糖凝集素9 (Gal-9)是先天性和适应性免疫的调节剂,具有促炎和抗炎功能,取决于其表达水平和细胞位置。然而,Gal-9在痛风性关节炎的发生和发展过程中调节炎症反应的具体细胞和分子机制尚未阐明。
在这项研究中,研究者通过监测原位中性粒细胞、单核细胞和Th17/Treg募集的表型和相关的细胞趋化因子谱来全面表征外源性Gal-9在MSU晶体诱导的痛风炎症模型中的功能作用。Gal-9治疗剂量依赖性地降低了关节炎症评分、膝关节水肿和不同促炎细胞趋化因子表达。此外,流式细胞术分析发现MSU晶体注射使募集到关节的白细胞总数显著上升,其中中性粒细胞(CD45+ /LY6-Ghi/ LY6-Chi)和单核细胞(CD11b+/CD115+/LY6-Chi)数量显著增加。Gal-9治疗后与MSU注射组相比,浸润性炎性单核细胞和中性粒细胞的百分比和绝对数量均显著下降。MSU注射的小鼠与对照相比总CD4+T细胞数量显著升高,与对照相比,Th17数量增加而Treg数量减少。Gal-9给药后,和Th17 (CD4+/IL-17+)/Treg (CD4+/CD25+/FOXP-3+)细胞比例显著降低。
总的来说,本研究中的结果表明,Gal-9的给药可以提供一种新的治疗策略,用于预防痛风性关节炎和其他基于炎症的疾病的组织损伤。
出处:
Front. Immunol., 28 October 2021 | https://doi.org/10.3389/fimmu.2021.762016

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#痛风性#
63
#ERS#
40
#Th17#
50
#Treg#
58
#乳糖#
41