ANGEW CHEM INT EDIT:南开大学团队成功提炼出对抗癌症新分子,抗癌活性史上强大
2017-10-26 佚名 Medicalxpress
一项新的研究显示,抗癌活性存在于类天然化合物循环缩肽类中,循环缩肽类是一种非常具有挑战性的结构。现在,中国科学家建立了一种合成化合物,专门针对胰腺癌干细胞,第一个阶段测试结果发表于《应用化学》杂志上。研究报告中特别指出,这是针对致命癌症的一次重大突破。
一项新的研究显示,抗癌活性存在于类天然化合物循环缩肽类中,循环缩肽类是一种非常具有挑战性的结构。现在,中国科学家建立了一种合成化合物,专门针对胰腺癌干细胞,第一个阶段测试结果发表于《应用化学》杂志上。研究报告中特别指出,这是针对致命癌症的一次重大突破。
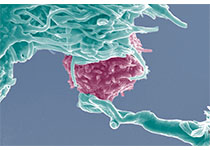
胰腺癌的癌细胞基本起源于干细胞,这些胰腺癌干细胞的耐药非常强,即使是最积极的治疗方案,效果也不太明显,因此寻找全新强大的药物组合是必不可少的。类天然化合物循环缩肽类肽环,包含着一个或多个肽酰胺,循环缩肽类在各种微生物中存在,如真菌、细菌、海洋生物等,大量证据证明它可以产生不同频谱生物活性,具有良好的抗癌效果。但是,一直以来,科学家们都找不到试验和研究所需要的材料,因此这种天然产物不仅罕见,而且很难孤立存在,想要将其合成需要非常复杂的化学结构。
如今来自天津南开大学分子药物研究重点实验室的研究人员们在这一领域取得了突破性进展,研究人员为这种缩肽类起了一个非常有技术含量的名字: 43547 - a2。该结构具有不同的部分,三个手性中心和两个双键,科学家们终于实现了15线性合成步骤。在试验过程中,研究人员发现这种化合物的抗癌活性超过了现有的所有抗癌药物。
原始出处:
Yuanjun Sun,Yahui Ding,Dongmei Li,et al, Cyclic Depsipeptide BE-43547A2 : Synthesis and Activity against Pancreatic Cancer Stem Cells, Angewandte Chemie International Edition (2017). DOI: 10.1002/anie.201709744
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#新分子#
27
#Angew#
30
#南开大学#
36
学习了.涨知识
47