冠脉CTA报告有规范标准啦!美国三大学会全新发布
2016-06-23 佚名 心在线
近日,美国心血管CT学会(SCCT)、美国放射学会(ACR)和北美心血管影像学会(NASCI),共同发布了一份新的报告制度,规范行冠状动脉CT血管造影(CTA)患者的报告。其称为冠状动脉疾病报告与数据制度(CAD-RADS),这一制度的发布将为全球数以百万计的患者带来一致性的冠脉CTA诊断信息。CAD-RADS规定了0(无狭窄)~5(至少一条动脉完全闭塞)的范围,根据分类进行进一步成像或处理。修饰
近日,美国心血管CT学会(SCCT)、美国放射学会(ACR)和北美心血管影像学会(NASCI),共同发布了一份新的报告制度,规范行冠状动脉CT血管造影(CTA)患者的报告。其称为冠状动脉疾病报告与数据制度(CAD-RADS),这一制度的发布将为全球数以百万计的患者带来一致性的冠脉CTA诊断信息。
CAD-RADS规定了0(无狭窄)~5(至少一条动脉完全闭塞)的范围,根据分类进行进一步成像或处理。修饰符S(支架)、G(移植)和V(易损斑块)用来更好地描述动脉。
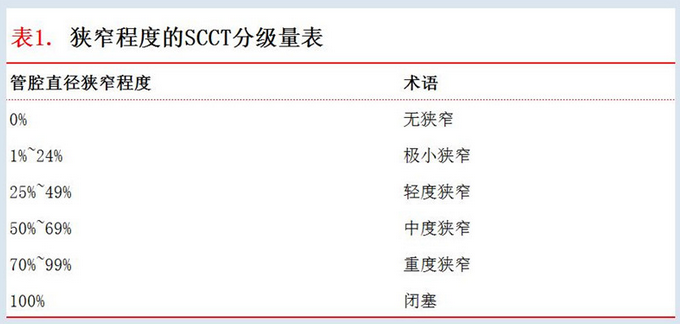
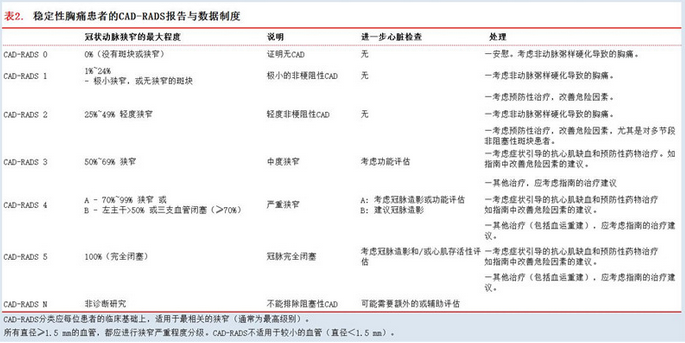
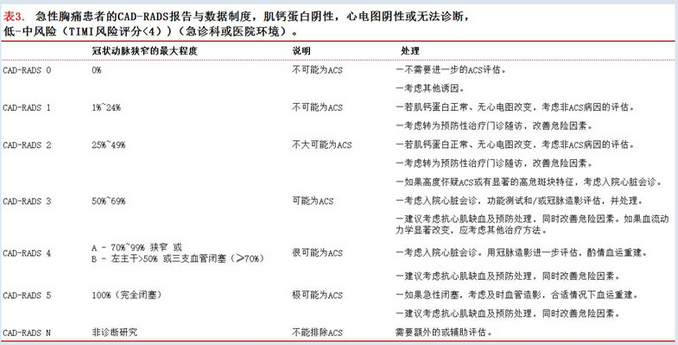
CAD-RADS分类取决于狭窄程度。SCCT建议分类系统为狭窄严重程度分级(表1)。表2和表3分别列出稳定性胸痛和急性胸痛的CAD-RADS报告制度分类。
图像示例:
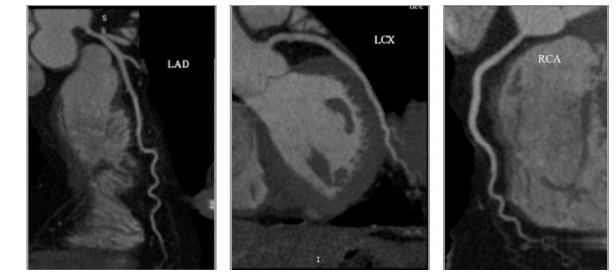
图 1. CAD-RADS 0:左主干正常,LAD、LCX和RCA无斑块或狭窄。

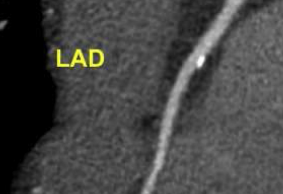
图 2. CAD-RADS 1:LAD近端极小的微钙化斑块,极小的管腔狭窄(狭窄直径<25%)。
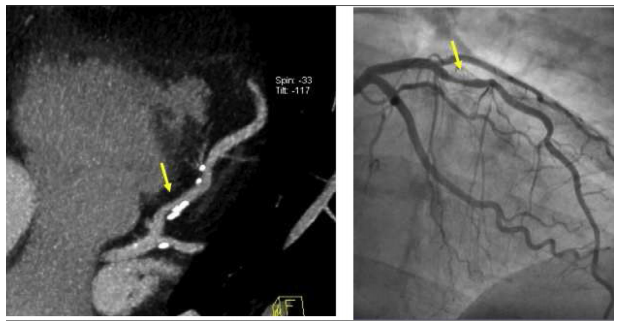
图3. CAD-RADS 2:主要钙化斑块在LAD近端,狭窄直径25%~49%(左)。冠脉造影证实25%~49%的狭窄(右)。
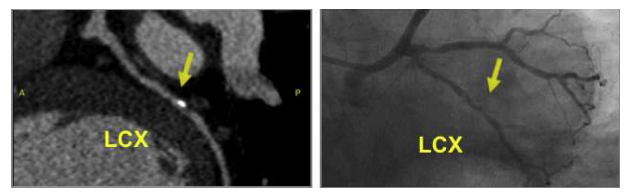
图4. CAD-RADS 3:主要钙化斑块在LAD中段,狭窄直径50%~69%。左图:冠脉CTA。右图:冠脉造影。
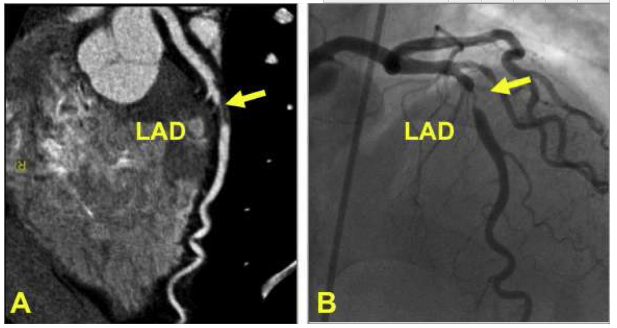
图5. CAD-RADS 4A:LAD中段非钙化斑块(黄色箭头),狭窄直径70%~99%(左)。冠脉造影证实LAD中段70%~99 %的狭窄(黄色箭头,右)。
 图6. CAD-RADS 4B:三支血管闭塞(狭窄>70%),包括RCA近端狭窄70%~99%(左),LAD近端狭窄70%~99%(中),LCX中段狭窄70%~99%(右)。
图6. CAD-RADS 4B:三支血管闭塞(狭窄>70%),包括RCA近端狭窄70%~99%(左),LAD近端狭窄70%~99%(中),LCX中段狭窄70%~99%(右)。
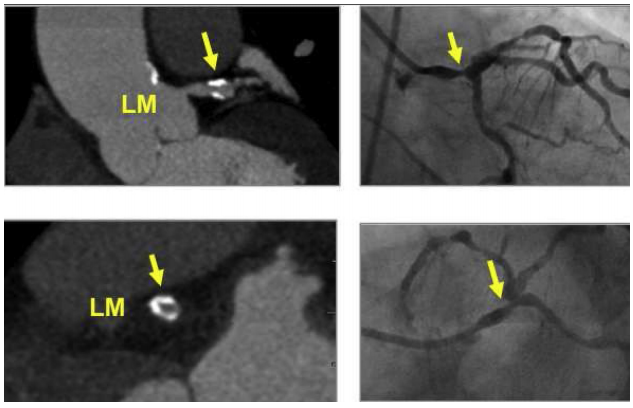
图7. CAD-RADS 4B:左主干远端环钙化斑块导致>50%的狭窄(箭头)。左上:左主干斜纵切面。左下:左主干远端横切面。右图:冠脉造影证实左主干远端严重狭窄。
 图8. CAD-RADS 5:左: RCA近端非钙化闭塞(箭头)。右:LCX近端全部闭塞(箭头)。LCX远端一个小的"孤立"钙化,支持慢性完全闭塞病变的诊断。
图8. CAD-RADS 5:左: RCA近端非钙化闭塞(箭头)。右:LCX近端全部闭塞(箭头)。LCX远端一个小的"孤立"钙化,支持慢性完全闭塞病变的诊断。
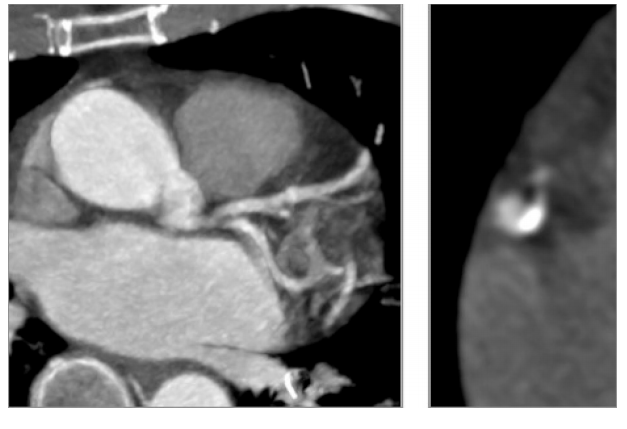
图9. CAD-RADS N:运动伪影遮盖了左主干、LAD和LCX,使这些部分不能诊断(左)。运动伪影在RCA中期(右)。RCA中段的运动伪影(右)。
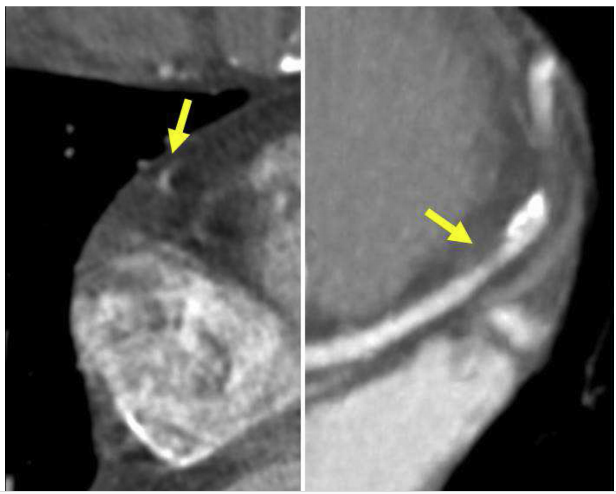
图10. CAD-RADS 3/N:运动伪影遮盖了RCA中段(左图,箭头),使这些部分不能诊断。LAD中段管腔狭窄50%~69%(右图,箭头),这部分病变符合CAD-RADS 3。虽然RCA中段不能诊断,LAD疑似闭塞应标记为CAD-RADS 3/N。若LAD轻度病变(直径狭窄<50%),未发现其他斑块,患者应标记为CAD-RADS N。

图11. CAD-RADS 4A/S:LAD近端支架内再狭窄,有显著管腔狭窄(狭窄70%~99%)。支架内再狭窄分级应遵循正常冠状动脉评分(0%狭窄,1%~24%狭窄,25%~49%狭窄,50%~69%狭窄,70%~99%狭窄,>99%狭窄)。在这种情况下,将严重的支架内再狭窄定义为CAD-RADS 4A病变。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习#学习#
86
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
87
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
97
很好,不错,以后会多学习
93
可以学习学习
101
#CTA#
41
#冠脉CTA#
39
#冠脉CT#
32