Sci Transl Med:真实的黑科技!“会变色文身”检测无症状的超早期癌症
2018-04-19 代丝雨 奇点网
文身,对大多数传统观念的人来说,应该已经与“社会”两个字绑定在一起了。但是你知道吗,文身也是可以用来治病的!
文身,对大多数传统观念的人来说,应该已经与“社会”两个字绑定在一起了。但是你知道吗,文身也是可以用来治病的!
目前发现最早的文身来自“冰人奥兹”,这具穿越了5000年时光的木乃伊身上具有多个文身,特别是在他的关节炎患处。这些文身的位置很多都与中医中的穴位不谋而合,因此也有人认为这是一种类似针灸的刺激疗法,可能用于治疗关节疾病和消化道疾病。
在随后的历史中,文身也被充满创意的科学家们用来治疗角膜浑浊、先天性血管痣,近来更是被应用在监测血液一氧化碳、葡萄糖等生理指标上。
本周的《科学转化医学》发布了一项最新研究,来自瑞士巴塞尔苏黎世联邦理工学院Martin Fussenegger教授团队,这位致力于哺乳动物细胞工程改造的大牛又带来了一项黑科技!将改造的工程细胞植入皮下,即可以对血钙浓度进行监测,如果出现高钙血症,细胞就会表达黑色素,使皮肤上出现一块“文身”!我们都知道,高钙血症与好多种癌症都是密不可分的,这种“文身”完全可以作为癌症出现的早期预警!
就像这样
钙本身就是一种细胞正常生理功能必须的元素,在维持细胞形态、细胞增殖分化等方面都有关键的作用。近来也有一些研究证实,钙粒子也与癌症的发展有关系。在正常的人体内,钙平衡受到精密的调控,当血钙降低,甲状旁腺激素即会开始运作,促进钙的再吸收和骨钙动员;当血钙过高,钙敏感受体(CaSR)则会被激活,抑制甲状旁腺激素的分泌。
但在肿瘤存在的情况下,原发肿瘤、转移肿瘤或者是它们吸引而来的免疫细胞,都会分泌多种体液因子,打破体内的钙平衡,最终导致高钙血症。
高血钙症状出现得很早,甚至可以在没有症状、或者没有典型癌症症状的时候就出现,所以科学家试图从这一点出发,通过监测血钙的变化来实现癌症的早诊早治。
具体用啥来监测呢?往回看两段,钙敏感受体!真是没有比这更天然、更灵敏的监测器了,实验数据也表明,钙敏感受体对轻微的高血钙(5.6-10mg/dl)就能产生响应,这正是很多无症状癌症患者的血钙浓度!
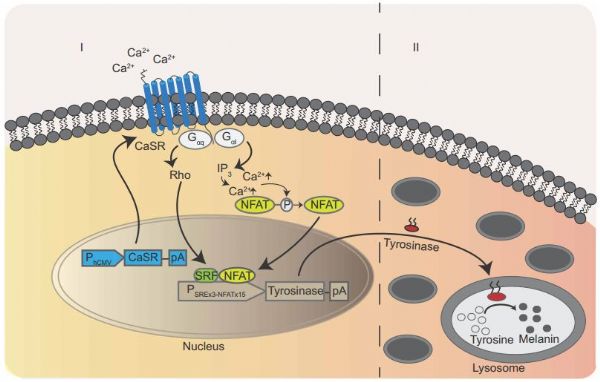
细胞改造思路
Fussenegger教授有丰富的改造细胞的经验,他很快设想出了一种可行的工程细胞。这种细胞将会表达钙敏感受体作为钙离子浓度监测装置,当监测到血钙离子浓度上升,细胞将启动下一步反应,通过激活酪氨酸激酶表达黑色素,如果顺利的话,黑色素的沉积将会形成一块肉眼可见的“文身”!
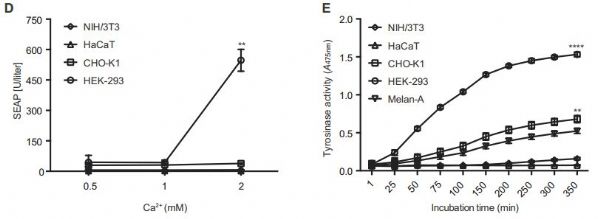
研究者们在几种不同的细胞系中尝试构建这种工程细胞,最终发现HEK293制成的成品是效果最好的,这种“文身细胞”对钙离子浓度变化敏感,下游黑色素的表达也比较灵敏,能够满足监测的需求。
HEK293效果是最好的
高钙粒子浓度下产生黑色素
研究者测试了一下文身细胞的实用性。毕竟人体内的各种生理指标都是动态平衡,没有哪个数值是一成不变的。如果血钙稍微升高了一点儿点儿它就报警,那也没法投入使用。
不过让研究者高兴的是,文身细胞稳健地证明了自己。在模拟轻微高血钙(1.6mM)和中度高血钙(1.8mM)的钙粒子浓度下,文身细胞都产生了足够肉眼观察的黑色素,而且要分别持续24小时和12小时才会出现明显的黑色素沉积。
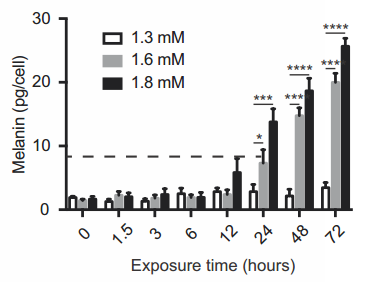
分别在12小时和24小时出现明显增长
而且,研究者还将形成的文身放在室温环境下观察了6个月,发现文身并没有随着时间流逝而消失,这说明文身还是很稳定的,并不那么容易被身体代谢掉。
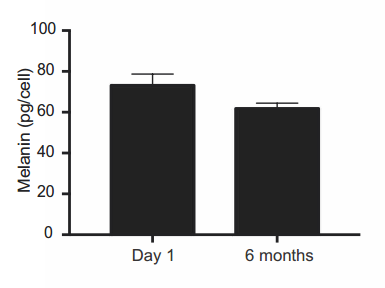
6个月内黑色素减少有限
接下来就是把文身细胞植入小鼠体内试一试了!为了方便观察,研究者选了没有毛发的裸鼠,在它们的身体一侧植入封装好的文身细胞,一侧植入不同肿瘤组织,有乳腺癌、结肠癌这样会造成高血钙的癌症,也有腺瘤这样与高血钙无关的。
结果令人激动啊,移植了高血钙相关肿瘤的小鼠都在植入位置上长出了一块文身,对照的小鼠则完全没有变黑的迹象!更令人激动的是,在实验进行的38天内,这些裸鼠可完全没有患病的迹象,都活泼得很呢!
对比很鲜明啊
可以说是超级激动啦~要是这种文身细胞在人体内也能够同样起效的话,那么它应该可以帮助高风险人群监测肿瘤发生,癌症就可以在很早的阶段被查出、被治愈啦~
当然,与高血钙相关的也不仅仅是癌症,还有甲亢、肉芽肿、认知障碍、肾衰等等疾病,这种细胞只能是作为一种辅助的筛查手段,具体确诊还是要看医生们的!
Fussenegger表示,这个思路不仅仅可以用在监测癌症上,它可以对任何生物标志物进行监测,将来这种文身细胞很可能会应用在许多缓慢进展的疾病上,例如神经退行性疾病。
原始出处:Aizhan Tastanova, Marc Folcher, Marius Müller, et al. Synthetic biology-based cellular biomedical tattoo for detection of hypercalcemia associated with cancer. Science Translational Medicine 18 Apr 2018.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#早期癌症#
27
#Transl#
33
#TRA#
27
#无症状#
26
#Med#
34
给力的检测手段 盼早日应用临床
50
谢谢分享学习
48