胸膜下线状影丨CT表现、诊断要点
2022-09-14 医学影像服务中心 熊猫放射
总体特征最佳诊断线索:平行于胸壁的胸膜下线发病部位:重力依赖,当患者改变体位时可消失大小:1-2mm厚的线,距肺边缘2-3mm形态学:线影远端的肺可透过度增强,远端肺也可不正常,形成带状影。
胸膜下线状影
Subpleural Linear Shadow
同义词:胸膜下线
影像表现
总体特征
-
最佳诊断线索:平行于胸壁的胸膜下线
-
发病部位:重力依赖,当患者改变体位时可消失
-
大小:1-2mm厚的线,距肺边缘2-3mm
-
形态学:线影远端的肺可透过度增强,远端肺也可不正常,形成带状影
CT表现
胸膜下线平行于胸壁
-
位于距肺边缘2-3mm范围内
-
上下范围可大于内外横向范围
-
远端肺可透过度增高:提示小气道阻塞并远端空气潴留,远端肺可以随体位改变恢复正常密度
-
远端肺可以为磨玻璃影,形成一条带状影而不是一条线影(称为坠积密度dependent density)
通常重力依赖
-
变为俯卧位后消失
-
纤维化不会消失
鉴别诊断
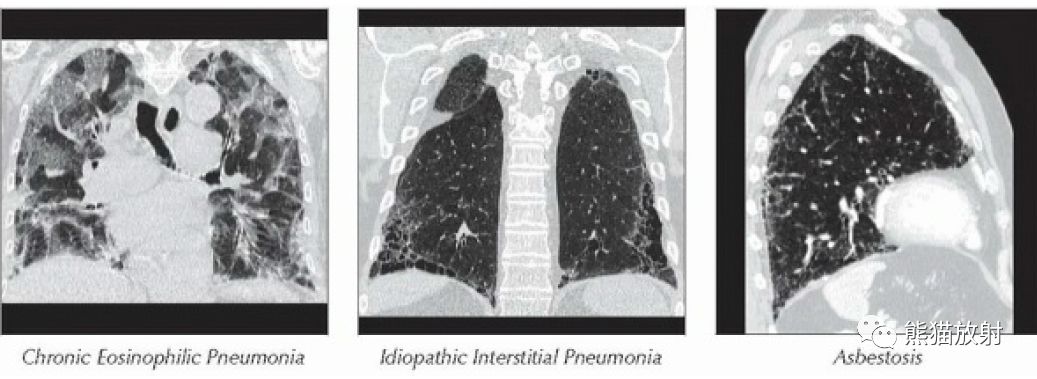
慢性嗜酸性粒细胞性肺炎
-
胸膜下线通常平行于胸壁
-
外周的实变由外向内:外周实变的吸收的内缘最后消失
-
上肺野常见,而非重力依赖
石棉沉着病
-
胸膜下阴影最初被描写为早期石棉沉着病的典型的改变
-
可能反映了石棉纤维在呼吸性细支气管内的沉积,引起小气道功能障碍
特发性肺纤维化
-
通常胸膜下为主
-
通常不是线影,蜂窝更常见
病理
总体特征
总体病理评述:最常见代表肺膨胀不全,但也可以代表纤维化
皮髓质肺
-
出现在肺“皮质”和“髓质”连接处
-
与大脑和肾相比,在肺内“皮质”和“髓质”无明确分界,除了血管大小不同
病因学
-
可以反映闭合气量与解剖的联系:由于老化(弹性减低)或小气道病变均可造成气道塌陷,肺容量改变。
大体病理及外科特征
-
肺边缘内2-3mm的位置是在次级肺小叶的小叶中央区的呼吸性细支气管的区域
临床表现
最常见体征/症状:通常无症状
年龄:随年龄增长发病率增高
自然病程及预后:可提示累及小气道的早期病变
诊断备忘
考虑:累及小气道的早期病变或正常老年人

横轴位HRCT示胸膜下曲线影与胸膜平行,位于下叶重力依赖区。注意线影远端的肺透亮区。

矢状位HRCT示胸膜下线的范围,位于背侧重力依赖区,线呈波浪状平行于胸膜走行。
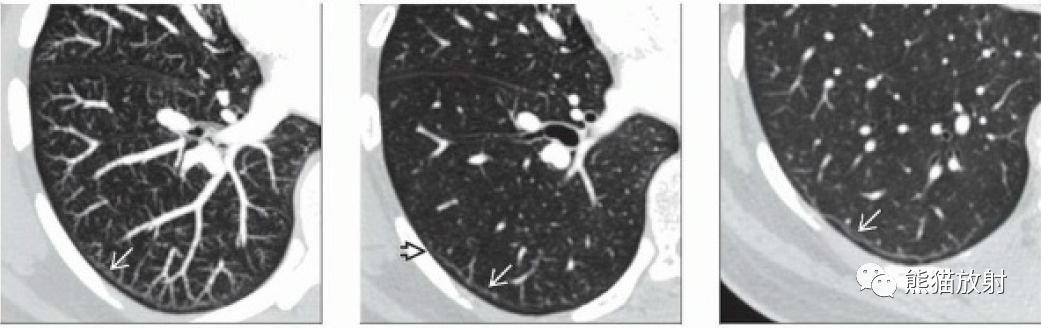
左图:横轴位HRCT MIP示胸膜下线及远端肺气肿,注意肺血管止于胸膜下线。
中图:横轴位HRCT示胸膜下线,注意在有些层面线影不完整。
右图:横轴位HRCT示胸膜下线为波浪形,注意线影的外侧较内侧显示好。
鉴别诊断:胸膜下肺
(慢性嗜酸性粒细胞性肺炎、特发性间质性肺炎、石棉肺)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#胸膜#
48
#诊断要点#
51
#CT表现#
49