GIE:伴HGD和IMC的Barrett食管行内镜治疗后再发浸润性腺癌的治疗
2014-03-04 佚名 丁香园
Barrett食管是一种癌前病变,可以进展为异型增生,甚至发展为食管腺癌。一旦Barrett食管发展为高度异型增生(high grade dysplasia,HGD)时,就有15%-60%的几率进展为腺癌。先前,食管切除术是治疗食管高度异型增生和腺癌的主要手段。目前,由于内镜技术的发展,普遍应用内镜下治疗(包括内镜下粘膜切除术和射频消融术)根除异型增生的Barrett食管和
Barrett食管是一种癌前病变,可以进展为异型增生,甚至发展为食管腺癌。一旦Barrett食管发展为高度异型增生(high grade dysplasia,HGD)时,就有15%-60%的几率进展为腺癌。先前,食管切除术是治疗食管高度异型增生和腺癌的主要手段。目前,由于内镜技术的发展,普遍应用内镜下治疗(包括内镜下粘膜切除术和射频消融术)根除异型增生的Barrett食管和部分粘膜内腺癌(intramucosal cancer,IMC)。
相比食管切除术,内镜下治疗表现出明显的优势:创伤小,最小化了手术操作相关的不良事件,保存了食管的正常生理结构。完全根除Barrett食管的标准是:新生的鳞状上皮细胞层替代肠上皮化生,根据不同的治疗方式,50%-90%的患者可以到达这样的治疗效果。目前,究竟有多少患者经过内镜治疗后会复发侵袭性食管腺癌,还缺乏相关资料。
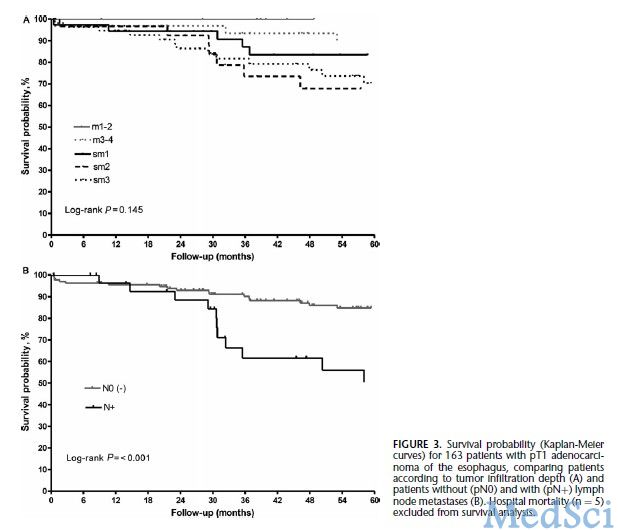
来自于华盛顿大学消化系统疾病研究中心的Adam Templeton等教授回顾了该中心194名经过内镜下或多种方式联合治疗的Barrett食管、高度异型增生或粘膜内腺癌的患者,经过审查委员会的批准进行了一项队列研究。该队列研究中,报道了4例经过内镜下治疗后复发浸润性腺癌的患者。4名患者中有3名完全根除了Barrett食管,随访时间为8个月到7年不等。
由3名内镜医生(A.R., S.I.G., S.I.)治疗所有患者的Barrett食管。最初用白光胃镜进行检查并按照西雅图协议行活检,用内镜下粘膜切除术(endoscopic mucosal resection,EMR)摘除结节性病变,内镜医生根据病情需要对部分患者进行共聚焦显微镜检查。组织学证实为高度异型增生或粘膜内腺癌的患者每3个月进行一次复查,发现结节性病变时通过EMR一并摘除。当白光胃镜未发现结节性病变时,通过射频消融术和氩离子凝固术(argon plasma coagulation,APC)根除可见的残余Barrett食管上皮层。按照2010年版TNM标准对病变进行分期。一旦内镜活检证实已成功根除Barrett食管,建议患者第1年内每6个月复查一次,之后每年复查一次。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#RET#
37
#内镜#
41
#Barrett食管#
43
#食管#
46
#内镜治疗#
45
#Barrett#
30