Cell Reports:LDL-C为癌转移重要因素
2014-05-15 高晓方 译 医学论坛网
澳大利亚一项研究表明,低密度脂蛋白胆固醇(LDL-C)为癌细胞转移的重要因素,胆固醇水平调节有望成为预防癌症转移的方法。论文发表于《细胞报告》(Cell Reports)。【原文下载】 远处转移为癌症的主要死因之一,深入了解癌症转移机制可显著改善癌症治疗。细胞表面粘附分子整合素有助于癌细胞脱离肿瘤并在其他部位定植,因此阻断整合素可防止癌细胞迁移和扩散,但目前研发的整合素抑制剂并不适用于临床。
澳大利亚一项研究表明,低密度脂蛋白胆固醇(LDL-C)为癌细胞转移的重要因素,胆固醇水平调节有望成为预防癌症转移的方法。论文发表于《细胞报告》(Cell Reports)。【原文下载】

远处转移为癌症的主要死因之一,深入了解癌症转移机制可显著改善癌症治疗。细胞表面粘附分子整合素有助于癌细胞脱离肿瘤并在其他部位定植,因此阻断整合素可防止癌细胞迁移和扩散,但目前研发的整合素抑制剂并不适用于临床。
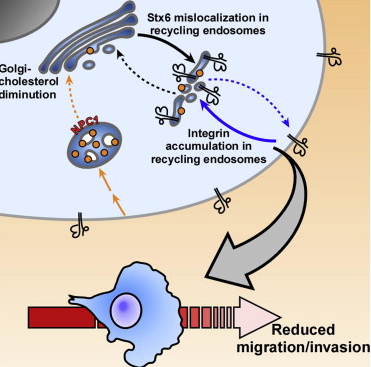
既往研究发现,整合素可由细胞表面迁移至细胞内,胆固醇则是将整合素保持在细胞表面的必需因素。此项研究表明,LDL-C可控制包括整合素在内物质运输,并且其对癌症细胞迁移和扩散能力具有显著影响。高水平LDL-C有助于癌细胞整合素移位至细胞表面,高水平HDL-C则可将整合素保持在细胞内。调节胆固醇水平有望成为影响癌细胞迁移和浸润的方法。
Reverter M1, Rentero C1, Garcia-Melero A1, Hoque M2, Vilà de Muga S1, Alvarez-Guaita A1, Conway JR3, Wood P2, Cairns R2, Lykopoulou L4, Grinberg D5, Vilageliu L5, Bosch M6, Heeren J7, Blasi J8, Timpson P3, Pol A9, Tebar F10, Murray RZ11, Grewal T12, Enrich C13.Cholesterol Regulates Syntaxin 6 Trafficking at trans-Golgi Network Endosomal Boundaries.Cell Rep. 2014 May 8;7(3):883-97. doi: 10.1016/j.celrep.2014.03.043. Epub 2014 Apr 17.【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CEL#
19
#Cell#
0
#LDL#
22
#癌转移#
17