Clin Gastroenterol H:停用英夫利昔单抗会增加UC患者复发风险
2016-10-08 xing.T MedSci原创
这个回顾性队列研究结果表明即使临床症状持续缓解的UC患者,停用英夫利昔单抗会增加UC患者复发风险,对复发患者重新开始治疗是有效和安全的。
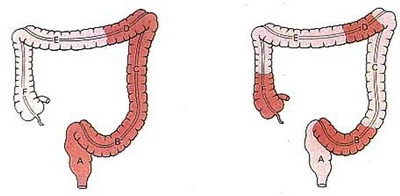
英夫利昔单抗是一种安全、有效的治疗溃疡性结肠炎(UC)的药物。近日,消化病领域权威杂志《Clinical Gastroenterology and Hepatology》发表了一项多中心回顾性队列研究结果,旨在明确经英夫利昔单抗治疗持续缓解的患者能否停药。
在这项回顾性队列研究中,研究者收集了13级转诊炎症性肠病中心所有接受英夫利昔单抗治疗的UC患者(n=193)的病历资料。研究者比较了临床症状缓解至少12个月而停用英夫利昔单抗的UC患者(n = 111)和继续预定的英夫利昔单抗治疗的UC患者(对照组,n =82)的病程长短,并且分析比较了停药后,不同治疗策略患者UC复发的发生率、住院和手术情况,并评估重新服用英夫利昔单抗患者的响应率和不良影响的缓解情况。
在整个队列中,67例(34.7%)UC患者在随访期间复发。停药组患者的复发率(23.3人/100人/年)明显高于对照组患者与对照组(7.2人/100人/年),在单因素分析中(对数秩P<0.001;风险比为3.41;95%置信区间为1.88–6.20)以及多变量分析中(风险比为3.70;95%可信区间为2.02–6.77),两组间住院及手术率没有显著差异。
这个回顾性队列研究表明:即使临床症状持续缓解的UC患者,停用英夫利昔单抗会增加UC患者复发风险,对复发患者重新开始治疗是有效和安全的。
原始出处:
Navarro Cortes,et al. Discontinuation of Infliximab in Patients With Ulcerative Colitis Is Associated With Increased Risk of Relapse: A Multinational Retrospective Cohort Study. clinical gastroenterology and hepatology 2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#AST#
31
#复发风险#
21
#GAS#
33
#Gastroenterol#
31
好文章,受益
56
继续关注!
67
谢谢分享!
67