LEUKEMIA:Erk1/2i 和 CDK4/6i 联合治疗复发难治性多发性骨髓瘤
2022-02-18 MedSci原创 MedSci原创
这项研究为 Erk1/2i + CDK4/6i 联合临床试验提供了临床前框架,以靶向 Ras+CDK 通路改善 MM 患者的预后。

尽管治疗取得了进展,但由于复发率高和耐药性的发展,复发性多发性骨髓瘤 (MM) 仍然无法治愈。MM 的复发和进展是由恶性浆细胞 (PC)内遗传变化的积累驱动的。目前已在 50% 的新发患者和 70% 的复发性多发性骨髓瘤 (MM) 患者中检测到致癌激活的 RAS 突变
最近的研究表明 Erk1/2 和 CDK4/6 抑制剂在转移性复发癌症中的高效力,一研究团队假设同时针对RAS / MAPK包括 Erk1/2 和 cyclin-Ds 在内的通路分子可增强 MM 细胞毒性并最大限度地减少副作用,他们使用 MM 的体外和体内临床前模型检查了 Erk1/2i、CDK4/6i 和 Erk1/2i + CDK4/6i 治疗效果。

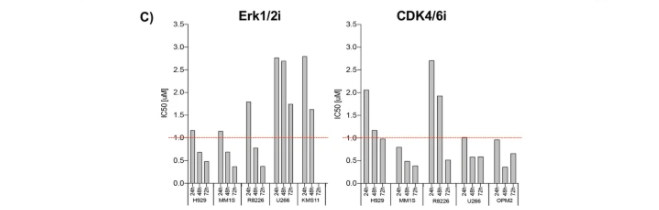
图 1:Erk1/2i + CDK4/6i 对 MM 细胞系和 HD-PBMC 的影响
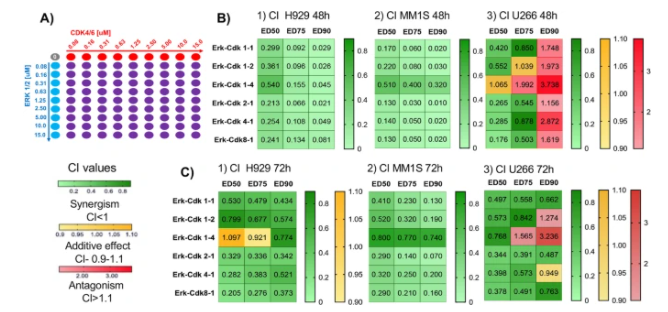
图 2:Erk1/2i + CDK4/6i 对 MM 细胞的协同细胞毒作用
他们的研究显示了 Erk1/2i + CDK4/6i 在 MM 细胞中的强协同 (IC < 0.5) 细胞毒性。Erk1/2i + CDK4/6i 以剂量依赖性方式处理使 MM 细胞处于 G0/G1 期并激活线粒体凋亡信号传导。

图 3:Erk1/2i + CDK4/6i 处理触发细胞周期停滞并诱导细胞凋亡
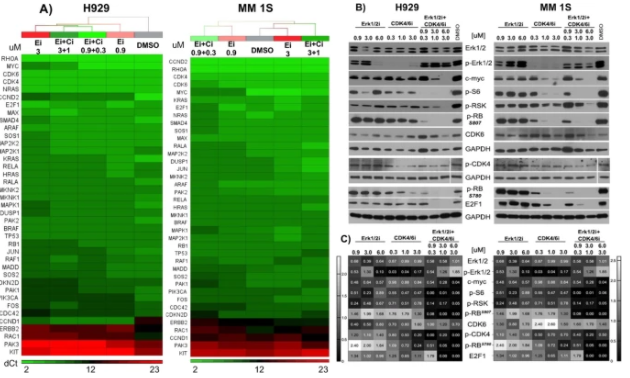
图 4:ERK1/2i + CDK4/6i 对 MM 细胞系中基因和蛋白质表达的影响

图 5:Erk1/2i + CDK4/6i 降低 MM1.S-Luc +异种移植体内模型中的肿瘤负荷。
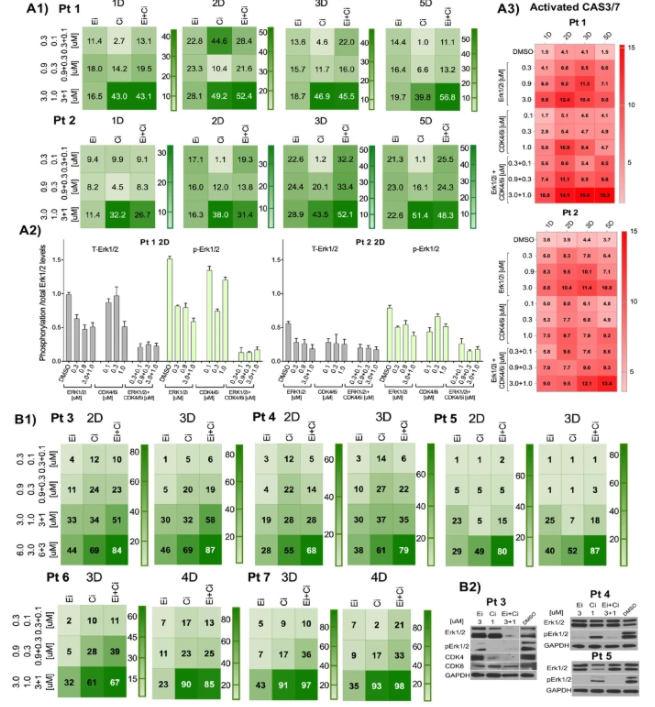
图 6:Erk1/2i 和 CDK4/6i 对原代 MM 细胞(A 1、B1、B3)的影响。
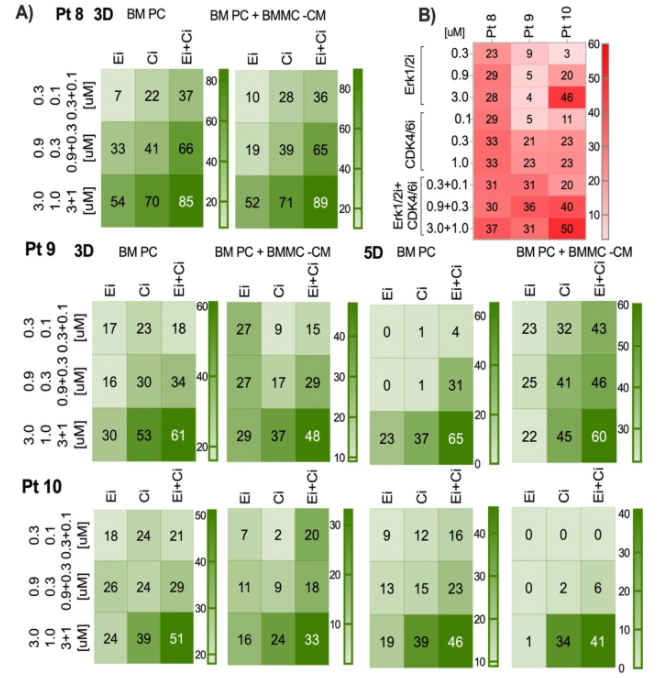
图 7:ERK1/2i + CDK4/6i 对与或不与 BMSC-CM 共培养的原代 MM 细胞的影响
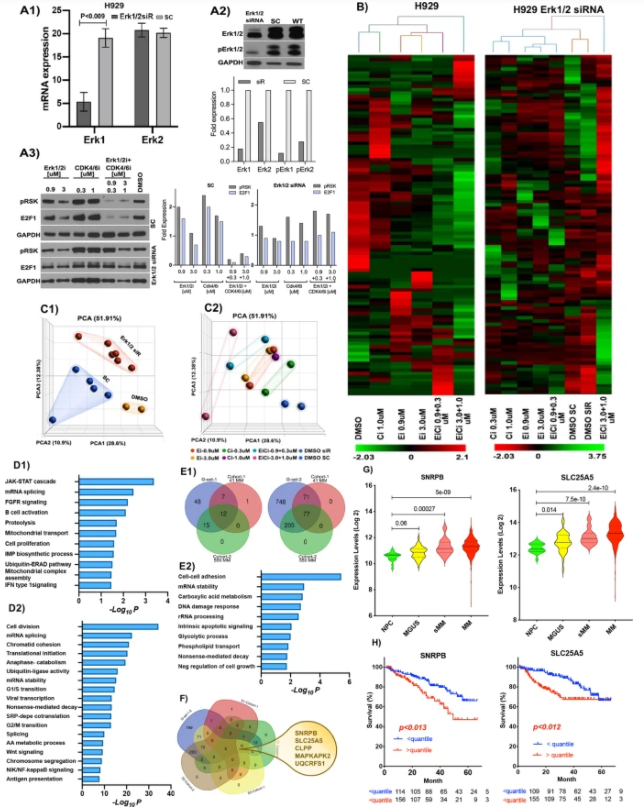
图 8:基于基因特征的方法确定了与 Erk1/2i + CDK4/6i 治疗相关的靶标
研究表明,Erk1/2i + CDK4/6i 治疗诱导抑制 Erk1/2 和 CDK4/6 信号传导中的关键靶分子,例如 c-myc、p-RSK、p-S6、p-RB 和 E2F1,表明了这些抑制剂的靶向活性。证明了联合疗法在广泛浓度下对遗传异质性和耐药性 MM 细胞系和患者细胞的协同细胞毒性。确定了与 Erk1/2i + CDK4/6i 治疗相关的基因特征,包括 SNRPB 和 SLC25A5基因,这些基因分别参与 RNA 加工和线粒体代谢。
总体而言,这项研究为 Erk1/2i + CDK4/6i 联合临床试验提供了临床前框架,以靶向 Ras+CDK 通路改善 MM 患者的预后。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#多发性#
35
#CDK4#
39
#复发难治#
35
#ERK#
53
#联合治疗#
42
#CDK#
32
#CDK4/6#
35
#难治性#
30
不错
59