JACC:可通过心动图识别心脏瓣膜病的深度学习模型
2022-08-11 MedSci原创 MedSci原创
通过对心电图进行深度学习分析,该模型可以准确地检测出AS、AR和MR,可以作为开发心脏瓣膜病筛查方案的基础
心脏瓣膜病是心血管疾病发病率和死亡率的一个重要因素,目前仍有大量患者未得到充分诊断。对心电图 (ECG) 进行深度学习分析可能有助于发现主动脉瓣狭窄(AS)、主动脉瓣反流 (AR) 和二尖瓣反流 (MR)。
该研究目的是开发ECG深度学习算法以识别单发和多发的中度或重度AS、AR和MR。
共纳入了于2005年-2021年期间进行心彩超检查前1年内进行过心动图检查的77163位患者,随机分至训练集(n=43165)、验证集(n=12950)和检验集(n=21048;7.8%的患者有AS、AR或MR)。采用受试者工作特征下面积 (AU-ROC) 和精确召回曲线评估模型表现。并在一个独立的数据集上进行外部验证。利用深度学习模型模拟筛选效果,利用不同疾病流行程度对测试精度进行建模。
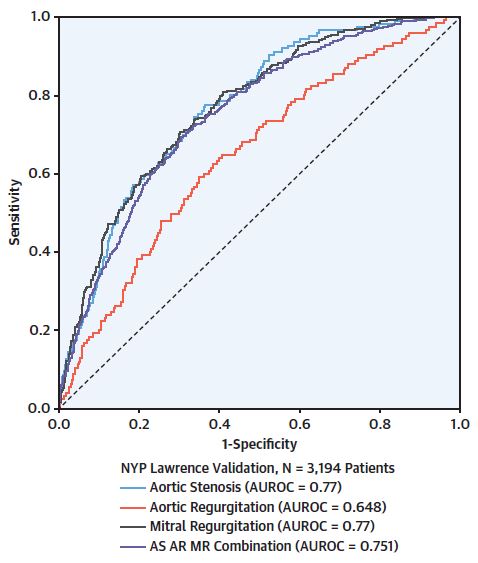
该模型在独立验证队列中的表现
该深度学习算法模型的精确度如下:AS (AU-ROC: 0.88),AR (AU-ROC: 0.77),MR (AUROC: 0.83) ,存在AS、AR或MR (AU-ROC: 0.84; 灵敏度 78%, 特异性 73%),在外部验证队列中有相似的精确度。在筛选程序建模中,试验特征依赖于潜在患病率和选定的敏感性水平。患病率为7.8%时,阳性预测值为20%,阴性预测值为97.6%。
总之,在该多中心队列研究中,通过对心电图进行深度学习分析,该模型可以准确地检测出AS、AR和MR,可以作为开发心脏瓣膜病筛查方案的基础。
原始出处:
Elias Pierre,Poterucha Timothy J,Rajaram Vijay et al. Deep Learning Electrocardiographic Analysis for Detection of Left-Sided Valvular Heart Disease.[J] .J Am Coll Cardiol, 2022, 80: 613-626. https://doi.org/10.1016/j.jacc.2022.05.029
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#深度学习模型#
118
学习
93
#心动图#
131
#JACC#
149
获益匪浅
168
#心脏瓣膜#
123
#心脏瓣膜病#
116
#ACC#
173
#瓣膜#
110