霉菌性脊柱炎1例并文献复习
2020-08-18 刘磊,张泉 国际医学放射学杂志
霉菌性脊柱炎(aspergillus spondylodiscitis,AS)是一种临床罕见的脊柱感染性疾病。AS多见于免疫缺陷的病人,通常继发于肺部、胃肠道或脑部霉菌感染,经直接播散或血源
霉菌性脊柱炎(aspergillus spondylodiscitis,AS)是一种临床罕见的脊柱感染性疾病。AS多见于免疫缺陷的病人,通常继发于肺部、胃肠道或脑部霉菌感染,经直接播散或血源性传播而引起,罕见发生于免疫功能正常的人。由于该病发生率较低,对其临床表现及影像特征认识不足,临床工作中误诊率较高。本文通过对1例AS病人的临床和影像表现、病理资料的回顾分析,并结合相关文献来了解AS的影像特点,以利于鉴别诊断。
1.临床资料
病人女,38岁,主诉背部疼痛6个月,加重伴双下肢麻木3个月,逐渐出现自足至腹部麻木症状,活动后加重,休息后好转,无夜间疼痛,无会阴部麻木,无大小便功能障碍,未行任何诊治。近半月出现盗汗。自发病以来,精神食欲可,体质量减轻,大小便正常。专科检查:胸4~胸7棘突及棘突旁压痛,胸椎活动受限。关键感觉点轻触觉:平剑突(胸7)以下感觉麻木。
实验室检查:白细胞:10.8×103[正常值(4~10)×103],中性粒细胞占比:75.5%(正常值40%~75%),血小板计数:462(正常值125~350),血沉:43mm(正常值0~20mm),C-反应蛋白:54.4mg/L(正常值<10mg/L),空腹血糖:8.3mmol/L(正常值3.9~6.1mmol/L),糖化血红蛋白:7.2%(正常值4.0%~6.3%),肝肾功能和肿瘤标志物均未见异常。
2.影像表现
胸椎CT显示胸4~胸7椎体骨质密度不均匀性增高,其内可见斑点状低密度影(图1A),椎体形态尚可,椎间隙无狭窄,软组织窗显示病变椎体周围可见软组织密度影(图1B)。MRI平扫显示胸4~胸8椎体可见多发斑片状异常信号影,T1WI上呈低信号,T2WI上呈稍高信号,抑脂序列呈高信号,相应水平椎管内硬膜外间隙可见软组织信号影,包绕脊髓,致使其轻度受压、向背侧移位,相应水平椎管明显狭窄,邻近椎旁软组织肿胀,纵径约为100mm。增强检查显示病变椎体、椎管内硬膜外及椎旁软组织肿块呈明显强化(图2、3)。
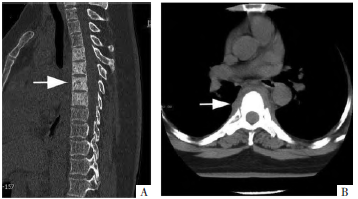
图1 胸椎CT平扫影像。A图,多平面重组示胸4~胸7椎体密度增高(白箭),其内可见斑点状低密度。B图,软组织窗示椎体周围软组织明显增厚(白箭)。

图2 全脊柱MRI影像。A图,T1WI示胸4~胸8椎体多发低信号影,椎旁及椎管内病变呈条状等信号影(白箭)。B图,短时反转恢复序列示胸4~胸8椎体多发高信号影,椎旁及椎管内病变呈高信号影(白箭)。C图,T1WI增强示胸4~胸8椎体病变、椎旁以及椎管内病变明显强化(白箭)。
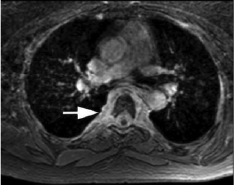
图3 脊柱横断面影像。T1WI增强示病变广泛累及椎旁和椎管内硬膜外间隙,包绕脊髓(白箭)。
3.手术与病理
病人行胸椎经后路内固定术+经右侧前方入路胸4~胸7椎体次全切椎管减压术,术中显示病变椎体骨质硬化明显,椎体后侧可见增生的瘢痕组织,切除脊髓前方瘢痕,显露脊髓,硬膜波动正常。病理学检查:HE染色可见肉芽肿样结构及大量多核巨细胞(图4A),PAS染色、六铵银染色均可见霉菌团(图4B、4C),抗酸染色阴性,病理诊断为霉菌感染。血清曲霉菌半乳甘露聚糖检测(GM试验)阳性:1.29μg/L(>0.85μg/L为阳性;<0.65μg/L为阴性;0.65~0.85μg/L时建议连续检测观察)。
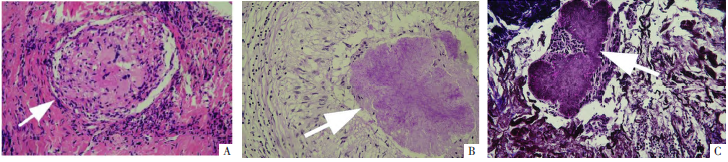
图4 病理图。A图,镜下可见肿物由大量多核巨细胞构成的肉芽肿样结构构成(白箭)(HE,×400)。B图,镜下可见肉芽肿样结构包绕的霉菌团(白箭)(PAS,×400)。C图,镜下可见霉菌团(白箭)(六铵银,×400)。
4.讨论
AS是临床罕见的真菌感染性疾病,在健康人群中罕见,绝大多数病人为免疫力缺乏或患有慢性疾病(艾滋病、器官移植、接受化疗或免疫抑制治疗)。Nicolle等分析了44例发生于免疫功能正常的AS病人,平均年龄48.85岁,男性多于女性,84%病人存在一定的诱发因素,包括肺部曲霉菌病、肺结核、椎间盘切除术、糖尿病、慢性阻塞性肺疾病和霉菌性心内膜炎等。本病例的实验室检查提示空腹血糖和糖化血红蛋白均超过正常范围,提示其存在糖尿病。
对于AS病灶,儿童通常由肺部病灶直接播散而来,成人多为肺部、胃肠道或脑部病灶经血源性传播而来。AS临床表现缺乏特异性,包括腰背痛、下肢无力和体质量减轻,如有硬膜外脓肿或肉芽肿形成,可出现脊髓神经受压的症状,甚至会出现截瘫。本病例以腰背痛和双下肢麻木为主要临床表现,其临床特点与文献报道一致。病人的白细胞和C-反应蛋白可以在正常范围内,对于AS的诊断价值不大。本病例的白细胞计数和C-反应蛋白均升高、血沉增加,提示感染性疾病的可能性大。
有研究表明血浆(1→3)-β-D-葡聚糖(BDG)和血清GM试验对于霉菌性脊柱炎的诊断有意义。本病例在手术病理证实为霉菌感染后进行了GM试验,结果为阳性。后经抗霉菌治疗后GM试验结果逐渐好转,并于出院前转变为阴性。但是AS的诊断仍依赖穿刺或者手术病理检查。经过手术和/或抗真菌治疗后,病人一般预后良好。
AS影像表现与病人的免疫状态以及病程时期有关。CT检查显示,病变早期椎体表面骨质吸收。进行期椎体出现蜂窝状或泡沫状骨质破坏区伴有边缘骨质硬化,随着病情进展,低密度区更为明显,椎间盘也可受累。病情好转时椎体骨质硬化明显,可致椎体增厚增宽,亦可见骨刺形成,有时可形成椎体压缩变形及椎旁脓肿。
MRI检查显示病变早期局限于椎体终板,随着病情进展,可累及整个椎体及其附件,形成椎旁及硬膜外肉芽肿或脓肿,T1WI上呈低信号,T2WI上呈等信号或稍高信号,抑脂序列呈高信号,增强检查呈明显强化。病程早期椎间盘不受累、椎间隙正常,晚期椎间盘可受累塌陷、椎间隙狭窄。Williams等研究认为T2WI上椎间盘信号不高、椎间隙存在是AS与化脓性脊柱炎的重要鉴别点。
需要与本病鉴别的脊柱病变主要包括:
①脊柱结核,以腰椎发病最多,胸腰段次之,可有低热、食欲差和乏力等全身中毒症状,常有肺结核病史,CT表现为椎体斑片状或虫蚀样骨质破坏,并可见死骨形成,骨质硬化不明显,椎旁脓肿和腰大肌脓肿形成,椎间盘破坏致椎间隙变窄,椎体前部压缩变扁,易造成脊柱畸形,较少累及附件,椎旁脓肿内可见条状、片状及砂粒样钙化。
②化脓性脊柱炎,起病急,出现剧烈的胸腰背部疼痛,伴有体温升高,病程相对较短;急性期椎体发生溶骨性破坏,破坏区内可见死骨形成,椎旁软组织肿胀、边界模糊,呈实性强化(以肉芽组织增生为主),椎间盘破坏快而明显,致使椎间隙变窄;慢性期,椎旁韧带增厚骨化,形成骨桥,骨质增生明显,累及的椎体数目一般较少,椎旁脓肿范围小,常不超过2个椎体高度。
③布氏杆菌性脊柱炎,牧区常见,临床表现为腰背部和腰骶部疼痛、活动受限,以多椎体、跳跃性发病为特征,影像表现为椎体邻近面骨质破坏合并骨质增生、硬化,相邻椎间隙变窄,未见椎旁及腰大肌脓肿。
④脊柱成骨性转移瘤,前列腺癌、乳腺癌和鼻咽癌等是常见的成骨性转移肿瘤,CT表现为斑点状或块状骨质硬化,常为多发,椎体广泛转移时,则整个椎体均匀性骨质硬化,可累及硬膜外间隙,但是形成椎旁软组织肿块者少见,椎弓根及附件常受累,椎间盘不受累。
⑤脊柱淋巴瘤,以非霍奇金淋巴瘤为主,多表现为单椎体或连续椎体侵犯,以溶骨性骨质破坏为主(单纯虫蚀型、浸润型或合并骨质硬化),伴周围软组织肿块形成,软组织肿块位于硬膜外且包绕病变椎体生长,椎间隙正常,增强检查肿瘤呈轻至中度强化。
原始出处:
刘磊,张泉.霉菌性脊柱炎1例并文献复习[J].国际医学放射学杂志,2019(02):223-226.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习了
52
#霉菌#
36
学习
93
#脊柱炎#
32
👍
109
!
88
👍
80