Nat Cell Biol:挑战常规!发现人肝细胞抵抗HCV感染的代谢过程
2016-10-15 佚名 生物谷
病毒感染是二十一世纪面临的主要医学挑战之一,从影响全球3%人口的丙肝病毒(HCV)流行病到最近爆发的西尼罗河病毒、寨卡病毒和埃博拉病毒感染。 病毒缺乏进行自我复制所需的基础代谢机制。为了解决这个问题,它们劫持它们的宿主的代谢机制以便完成它们的生命周期和进行增殖。然而,科学家们仍然并没有很好地理解病毒与它们感染的有机体之间在代谢上的相互作用。这主要是因为人基因与代谢过程之间存在复杂的相互作用。
病毒缺乏进行自我复制所需的基础代谢机制。为了解决这个问题,它们劫持它们的宿主的代谢机制以便完成它们的生命周期和进行增殖。然而,科学家们仍然并没有很好地理解病毒与它们感染的有机体之间在代谢上的相互作用。这主要是因为人基因与代谢过程之间存在复杂的相互作用。
如今,在一项新的研究中,来自以色列、美国、意大利和德国的研究人员系统性地鉴定出一组控制对HCV感染作出的代谢反应的基因开关。通过仔细地选择靶向这些基因开关的药物,他们能够发现这些基因如何控制代谢过程,如葡萄糖和脂质代谢,并且建立这些过程如何影响这种病毒的生命周期。令人吃惊的是,尽管一些代谢过程对这种病毒是有利的,比如通过给它提供允许它快速增殖的用于构建它的遗传物质的构成单元(building block),但是其他的代谢过程却是抗病毒的,会干扰这种病毒的生命周期。
论文通信作者、以色列耶路撒冷希伯莱大学亚历山大-格拉斯生物工程中心主任Yaakov Nahmias教授说,“这首次表明我们的细胞能够阻断HCV和寨卡病毒等黄病毒科复制,阻断方式是阻止它们获得它们存活所需的至关重要的构成单元。我们的结果提供一种新的方法来治疗病毒感染:靶向对病毒依赖的代谢过程进行的基因调节。”
核受体
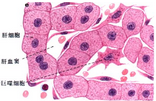
代谢是一种复杂的现象,主要是由被称作核受体的基因开关所调节的。核受体是一类在细胞内发现的能够被脂肪酸和葡萄糖等代谢物激活的蛋白,通过调节上百种基因表达(即激活)而允许细胞检测营养物变化(如吃早餐)并针对这种变化作出反应。
HCV等病毒能够干扰这种代谢调控。当这发生时,它会导致被感染的人患上脂肪肝和糖尿病。
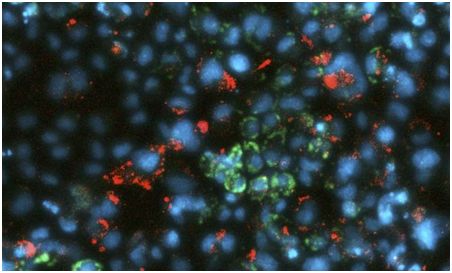
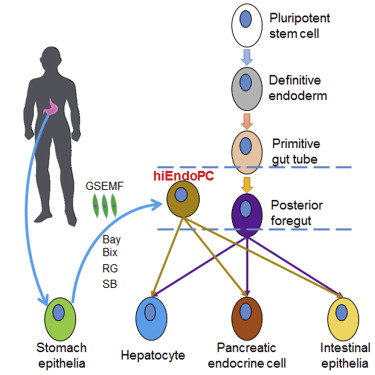
为了发现HCV等病毒能够干扰代谢调控的机制,研究人员利用一种新的由Nahmias开发的人肝细胞实验室模型开展研究。通过绘制被感染的肝细胞和正常的肝细胞的代谢图,他们能够着重关注受到干扰的代谢过程,并且鉴定出导致它们的调节异常的核受体。
一旦研究人员鉴定出控制受到干扰的代谢过程的基因开关,他们就利用药物阻断每个核受体,并且研究这种抑制对HCV的影响。尽管阻断葡萄糖代谢对HCV是有害的,但是阻断脂质代谢会产生相反的效果,事实上会增加HCV增殖。这些发现也在一小群HCV感染者体内得到验证。
研究人员指出包括HCV、登革热病毒、西尼罗河病毒、黄热病毒和寨卡病毒在内的黄病毒科病毒之前被认为是老练的代谢工程师,能够优化对宿主代谢机制的劫持从而产生更多的病毒。论文共同作者、德国杜塞尔多夫大学病毒学研究所科学家Jörg Timm教授说,“非常令人吃惊地观察到人肝细胞能够利用代谢过程抵抗病毒感染。这违反了我们将病毒作为老练的代谢工程师的常规理解,从而提示着靶向病毒感染的新途径。”
Gahl Levy, Naomi Habib, Maria Angela Guzzardi, Daniel Kitsberg, David Bomze, Elishai Ezra, Basak E Uygun, Korkut Uygun, Martin Trippler, Joerg F Schlaak, Oren Shibolet, Ella H Sklan, Merav Cohen, Joerg Timm, Nir Friedman & Yaakov Nahmias.Nuclear receptors control pro-viral and antiviral metabolic responses to hepatitis C virus infection.Nat Cell Biol.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肝细胞#
29
#Biol#
23
#Nat#
20
#CEL#
30
#Cell#
25
#HCV#
32
#HCV感染#
35
#Bio#
20