JAHA:老年人心脏结构和功能与糖尿病相关的死亡或心力衰竭风险的关系
2022-03-08 MedSci原创 MedSci原创
在老年人的混血儿队列中,心脏结构和功能异常部分解释了与糖尿病相关的事件风险增加。
即使在考虑了已知的心血管危险因素后,糖尿病与心力衰竭(HF)和死亡率的风险增加相关。与血糖异常相关的心脏结构和功能异常是否足以解释升高的死亡或心力衰竭(HF)风险仍未明确。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员分析了参加社区动脉粥样硬化风险(ARIC)研究中第5次随访评估(2011-2013年)的6059名参与者(平均年龄为75±5岁;58%为女性;22%为黑人)。
参与者分为无糖尿病、糖尿病前期和糖尿病(根据病史和糖化血红蛋白值来确定)三大类。研究人员评估了糖尿病是否改变了心脏结构和功能的超声心动图指标与全因死亡或心衰住院复合结局之间的关联,然后,研究人员估计了与糖尿病相关的复合结局风险增加的程度,主要通过心脏结构和功能来解释。
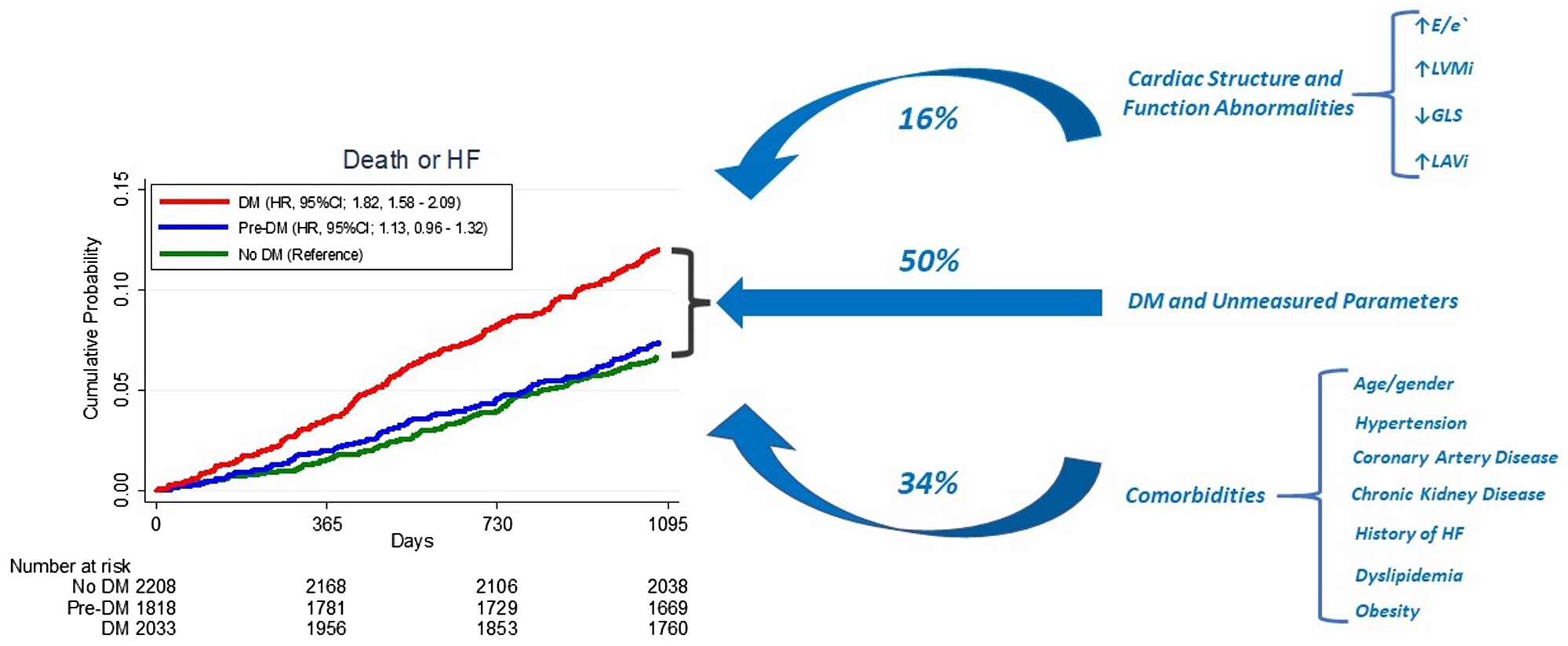
33.5%的受试者患有糖尿病。1111人(18%)发生死亡或心衰,每100人每年有3.6人死亡。在考虑了临床混杂因素后,心脏结构和功能以及糖尿病状态的指标均与较差的预后显著相关。虽然糖尿病始终与较高的事件风险相关,但它并没有显著改变心脏异常与死亡或心衰风险之间的关联,除了具有较高事件相对风险的左心房容积较高的受试者外(交互作用的P<0.001)。心脏结构和功能指标占与糖尿病相关的死亡或心衰风险增加了16%。在分析没有患有心脏病的受试者时,研究人员观察到了类似的结果。
由此可见,在老年人的混血儿队列中,心脏结构和功能异常部分解释了与糖尿病相关的事件风险增加。
原始出处:
Riccardo M. Inciardi.et al.Cardiac Structure and Function and Diabetes‐Related Risk of Death or Heart Failure in Older Adults.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.022308
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#风险的关系#
49
非常有用#心血管#
82
#AHA#
42
#心脏结构#
63