Oral Dis:研究证实牙周炎和银屑病之间存在正相关关系
2022-04-11 MedSci原创 MedSci原创
牙周炎是一种由细菌感染引发的慢性炎症性疾病,它激活了宿主的免疫反应,最终会导致牙齿脱落。牙周炎被认为是由口腔微生物群落与宿主反应的复杂相互作用造成的,并由遗传和环境因素改变。
牙周炎是一种由细菌感染引发的慢性炎症性疾病,它激活了宿主的免疫反应,最终会导致牙齿脱落。牙周炎被认为是由口腔微生物群落与宿主反应的复杂相互作用造成的,并由遗传和环境因素改变。银屑病是一种表现在皮肤或关节或两者的系统性炎症疾病,尽管其发病机制仍未被完全理解,但现在已认识银屑病的皮损起源于宿主免疫系统与常驻皮肤细胞类型相互作用失调的结果。由于银屑病和牙周炎有相似的致病机制,研究人员进行了一项荟萃分析以探究二者之间的关联。
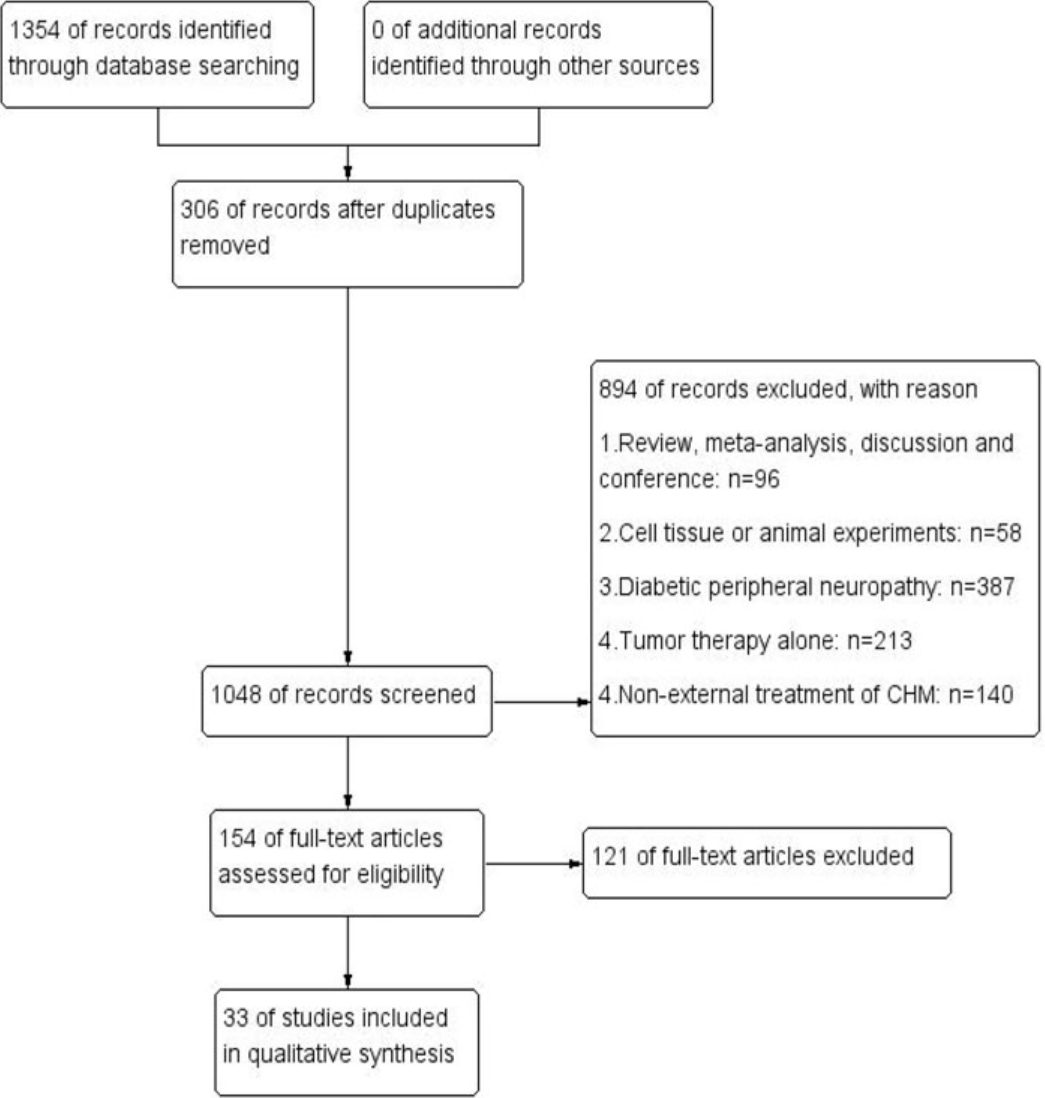
研究人员检索了三个数据库(MEDLINE、Embase和Cochrane图书馆),截止至2020年3月发表的评估牙周炎和银屑病之间关系的病例对照或队列研究。通过meta分析进行定量综合。
结果,研究共纳入了13项评估牙周炎和银屑病之间关系的研究(包括11项病例对照和2项队列研究)。在这13篇文章中,有9篇文章报告了牙周炎或银屑病的患病率。因此,对纳入的9项研究的数据进行了meta分析。9项研究的汇总效应结果显示,牙周炎患者与银屑病的风险较高,汇总OR为2.87(95% CI,1.75-4.69)。

综上所述,该系统回顾表明,牙周炎和银屑病之间存在正相关关系;但是,不能确定二者之间存在因果关系。由于证据不足,在解释有关牙周参数的结果时应慎重。有必要进行精心设计的前瞻性研究以评估两种疾病之间的相互作用。
原始出处:
Xinze Zhang, et al., Periodontitis in patients with psoriasis: A systematic review and meta-analysis. Oral Dis. 2022 Jan;28(1):33-43. doi: 10.1111/odi.13617.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oral#
28
#Dis#
33
#正相关#
36
#相关关系#
38
#牙周#
38