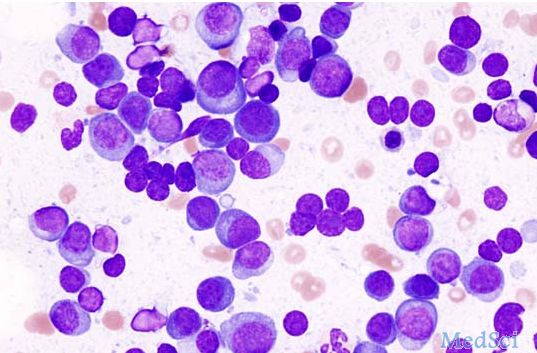
ASCO 2016:来那度胺维持疗法或可明显改善多发性骨髓瘤患者的存活率
2016-06-06 佚名 生物谷
目前很多临床试验都表明,利用药物来那度胺进行的维持疗法可以降低多发性骨髓瘤患者的疾病进展风险,然而在改善患者总体生存率上目前却并没有确定的研究结论。此前有很多研究发现,在自体造血干细胞移植后进行来那度胺维持治疗或可改善新诊断多发性骨髓瘤患者的总体生存率,而其它多发性骨髓瘤患者却并未因此获益,相关研究发表于近日举办的2016年美国临床肿瘤学会年会上。这项研究中,研究者对CALGB、IFM及GIMEM
目前很多临床试验都表明,利用药物来那度胺进行的维持疗法可以降低多发性骨髓瘤患者的疾病进展风险,然而在改善患者总体生存率上目前却并没有确定的研究结论。
此前有很多研究发现,在自体造血干细胞移植后进行来那度胺维持治疗或可改善新诊断多发性骨髓瘤患者的总体生存率,而其它多发性骨髓瘤患者却并未因此获益,相关研究发表于近日举办的2016年美国临床肿瘤学会年会上。
这项研究中,研究者对CALGB、IFM及GIMEMA进行的三项随机对照试验进行综合分析,研究包括1200多名参与者;其中有605名新诊断的多发性骨髓瘤患者,这些患者在自体造血干细胞移植后进行来那度胺维持治疗,同时对照为604名接受安慰剂或不进行维持治疗的患者,7年后研究者发现,进行来那度胺维持治疗的患者中有62%的患者存活着,而对照组中有50%的患者存活着,同时患者总体生存率在各研究组中基本一致。
研究者McCarthy说道,自体造血干细胞移植后进行来那度胺维持治疗被认为是一种治疗多发性骨髓瘤的标准疗法,过去十年里这种疗法明显改善了多发性骨髓瘤患者的生存率和生活质量,而且相关的研究结果也让研究者非常激动。
原始出处:
Roswell Park Cancer Institute.Lenalidomide maintenance therapy improves overall survival for patients with multiple myeloma.June 4, 2016
拓展阅读:与多发性骨髓瘤相关的拓展阅读:
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#ASC#
32
#存活率#
0
#多发性#
24