慢性肾脏病微血管内皮细胞损伤机制
2016-12-29 国际移植与血液净化杂志 国际移植与血液净化杂志
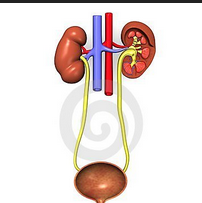
慢性肾脏病(CKD)在中国人群中的患病率为10.8%。肾脏内皮细胞(ECs)损伤已被证实与CKD进展密切相关。本文就慢性肾脏病微血管内皮细胞损伤机制研究进展进行了系统性阐述。内皮细胞损伤与肾脏疾病的关系肾脏微血管损伤与大部分肾脏疾病相关,微血管ECs损伤可能是肾小球进行性丢失不可逆损伤的起始因素。持续损伤使肾小管周围毛细血管(PTC)ECs开始凋亡,导致PTC结构和功能破坏,进而加重肾脏纤维化
慢性肾脏病(CKD)在中国人群中的患病率为10.8%。肾脏内皮细胞(ECs)损伤已被证实与CKD进展密切相关。本文就慢性肾脏病微血管内皮细胞损伤机制研究进展进行了系统性阐述。
内皮细胞损伤与肾脏疾病的关系
肾脏微血管损伤与大部分肾脏疾病相关,微血管ECs损伤可能是肾小球进行性丢失不可逆损伤的起始因素。持续损伤使肾小管周围毛细血管(PTC)ECs开始凋亡,导致PTC结构和功能破坏,进而加重肾脏纤维化进展。
多种肾脏疾病与肾小球内皮细胞(GEnCs)损伤直接相关,如GEnCs损伤是重度子痫前期肾脏损伤的中心环节;在ANCA相关性血管炎肾损害中也观察到GEnCs被直接损伤;人类白细胞抗原在肾脏ECs中广泛表达,移植肾病及艾滋病患者肾损害中,肾脏ECs是各种免疫球蛋白及HIV-1病毒的首要攻击目标,免疫反应调节物直接接近ECs表面,在急性排斥反应中是最严重的变化。
内皮细胞损伤相关因素
氧化应激
氧化应激产生大量活性氧(ROS),ROS可与一氧化氮(NO)快速结合,形成活性氮(RNS),产生亚硝化应激,增加ROS的促炎作用;ROS可通过氧化细胞关键通路蛋白加重ECs功能障碍,还可以氧化组成细胞的蛋白质和脂肪,破坏DNA,在糖尿病肾病(DN)及急性缺血性肾损害中参与ECs损伤和凋亡。不对称二甲基精氨酸(ADMA)是内皮型NO合酶(eNOs)的内源性抑制剂,氧化应激诱导可形成ADMA的S-腺苷甲硫氨酸-依赖蛋白精氨酸甲基转移酶产生,导致eNOs解偶联,促进内皮间充质转化;而辅因子四氢生物蝶呤(BH4)可通过稳定eNOs二聚体来维持eNOs系统的完整性,BH4氧化失活等造成BH4的缺乏可引起eNOs解偶联;eNOs减少引起NO缺乏,扩大局部炎症,造成ECs损伤。NOX4曾被称为肾NADPH氧化酶,脂多糖依赖NOX4的活化刺激ECs表达细胞间粘附分子(ICAM-1)等,NOX4活化也是DN的危险因子。
缺氧
缺氧诱发肾脏产生多种反应,分子水平上最重要的适应阶段由缺氧诱导因子(HIF)介导。HIF-1α通过直接或间接的方式调节超过2%的血管ECs基因,缺氧及HIF-1可调节与细胞周期和DNA复制有关的基因,刺激ECs增生和分化。HIF-2α的持续缺乏导致ECs与细胞外基质蛋白黏附减少。HIF-1α在多发性骨髓瘤患者中是增加的,且与血清β2微球蛋白水平明显相关,而β2微球蛋白的增加使肾单位负荷加重,其对PTC ECs的影响尚不明确。
血管生成素(Ang)
Ang-1具有稳定血管ECs功能,并受到Ang-2的拮抗。Ang-2通过收缩肾小球出球小动脉、增加转化生长因子-β(TGF-β)使肾脏缺氧加重。Ang-2可活化NADPH氧化酶诱导氧化应激,导致NO消耗,氧气利用率下降,而氧化应激、缺氧在ECs损伤过程中起关键作用。Ang-2还可触发ECs间充质转化,使ECs具有间质细胞特征。有人类Ang-2 1型受体( hAT1)过表达的转基因小鼠出现明显的蛋白尿,其足细胞表达hAT1尤其显著,说明Ang-2可能直接损伤足细胞。
血管内皮细胞生成因子(VEGF)
VEGF可增加细胞间转运以及ECs间隙的形成,促使ECs形成窗孔结构并维护其功能。ECs的完整性是通过细胞间隙大小的调节来维持的,而这个过程由Rho-A和Rac-1的活性变化严格调控。Rho-A激活诱导肌动蛋白和肌球蛋白收缩,增加ECs通透性;Rac-1通过增加邻近ECs之间的VE-钙黏蛋白黏附链接的保护减少ECs通透性。硫酸乙酰肝素蛋白多糖(HSGP)在肾小球ECs表达,是肝素结合生长因子、VEGF-A的受体,吞噬HIV的ECs释放HIV-1转录反式激活因子(Tat)蛋白,具有肝素结合生长因子功能,VEGF-A和细胞外的Tat与HSGP结合,相互协作改变Rho-A和Rac-1活性,调节HIV阳性儿童肾脏ECs骨架结构和通透性。
小板反应蛋白-1(TSP-1)
TSP-1是一种血管形成抑制剂,可抑制VEGF介导的ECs增殖,在肾脏血管ECs中有表达,巨噬细胞源性的细胞因子抑制局部VEGF产物的同时可刺激TSP-1的表达。CD148是在血管ECs表面表达的跨膜蛋白酪氨酸磷酸酶,在减少生长因子信号和抑制细胞增生方面有很重要的作用。TSP-1是CD148重要的功能性配体。
转化生长因子-β(TGF-β)
TGF-β与TGF-βⅡ型受体结合使TGF-βⅠ型受体磷酸化,活化的TGF-βⅠ型受体激酶使Smad2/3磷酸化,Smad2/3与细胞核结合并且调控基因表达,抑制ECs增生、迁移和血管管腔形成。
高血糖
高血糖以及因高血糖引起的代谢紊乱可通DAG/PKC通路、多元醇途径、TGF-β信号通路等途径损伤ECs。转谷氨酰胺酶(TG2)在细胞死亡、增生、分化和迁移过程中有很重要的作用。研究表明,高血糖可引起ECs内高钙,高钙通过活化PKC和NADPH氧化酶诱导ROS增加,ROS诱导ECs TG2活化,导致ECs凋亡。给予链脲霉素糖尿病小鼠模型C肽替代治疗后,C肽可保护糖尿病小鼠肾脏ECs。高血糖还可增加晚期糖基化终末产物(AGEs),上调AGEs受体,AGEs可诱导DN中ECs间充质转化,其中ECs表面的AGEs受体—Smad-3通路起关键作用,Smad-3特异性抑制剂可抑制Smad3磷酸化,为DN肾脏纤维化的治疗提供新思路。
肿瘤坏死因子(TNF)
肾脏几乎所有细胞(包括系膜细胞、足细胞、ECs、小管细胞)都能产生TNF-α,高糖和AGEs可能诱导肾脏细胞合成TNF-α。TNF-α上调ECs表面黏附分子的表达,介导其与单核细胞、淋巴细胞等的黏附,活化ECs使之迁移。TNF在脂多糖诱导的急性肾损伤模型中通过ECs的TNF受体1损伤肾脏ECs。有研究表明,TNF通过Rho/MLCK依赖性途径减少GEnCs表面的多糖蛋白复合物,增加细胞间间隙,改变ECs骨架结构及其通透性。
内皮细胞与周围细胞
GEnCs损伤可能与足细胞损伤有关,上皮细胞下沉积的细胞外基质使毛细血管壁增厚,影响足细胞与GEnCs之间的相互作用,也可能影响GEnCs在维持血流稳定方面的功能。系膜细胞免疫复合物引起炎症介质的形成和活化(如ROS、前列环素、血小板活化因子、TNF-α、集落刺激因子1、白细胞介素-6、趋化因子等),这些物质可以破坏内皮屏障,使更多的大分子达到肾小球系膜区,进一步增加炎症介质的产生,形成恶性循环。周细胞与ECs关系密切,可调节血管生成、稳定、成熟和重塑,在ECs的存活过程中有重要的生物学作用。
各种理化因素及内皮细胞周围细胞的影响均可导致肾脏ECs结构破坏和功能紊乱。ECs损伤在肾脏疾病中占有一定地位。研究CKD中肾脏ECs损伤对探索肾脏疾病进展其有重要意义,且能为延缓肾脏疾病进展提供新思路。
文章摘自:慢性肾脏病微血管内皮细胞损伤机制研究进展.国际移植与血液净化杂志, 2016,14(04): 21-23.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#血管内皮细胞#
32
文章不错,值得学习
56
#微血管#
33
#损伤#
34
#慢性肾脏#
28