Stroke:收缩压变化轨迹与急性脑出血患者预后的相关性
2022-06-09 MedSci原创 MedSci原创
收缩压从210mmHg以上降至140mmHg以下的急性脑出血患者3个月时的死亡或残疾和急性肾损伤的风险最高
在急性脑出血患者中经常观察到血压(BP)升高。既往研究表明,早期使用抗高血压药物降低血压有可能可降低血肿变大和神经功能恶化的风险。
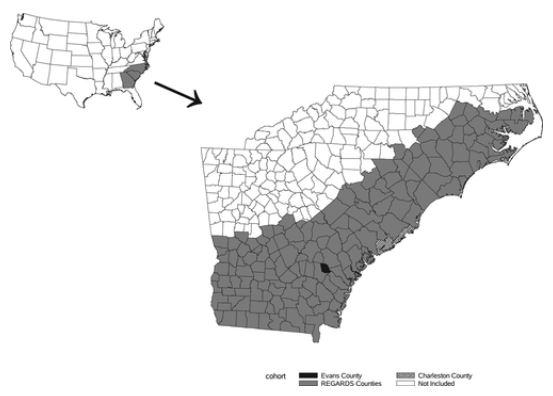
ATACH-2试验(急性脑出血的降压治疗-2)是一项国际性、随机化、2-组、开放标签的临床试验,旨在明确快速降低血压在急性自发性脑出血患者中的作用。本文汇报了在该试验中急性瞬时血压变化的异质性,及其与脑出血预后的相关性。
在该试验中,2011年至2015年期间,1000位急性脑出血患者被随机分至强化降压组(收缩压降至110-139mmHg)或标准降压组(140-179mmHg),所有患者通过静滴尼卡地平降压。研究人员采用基于组的轨迹建模分析了这1000位患者随机分组后24小时内每小时收缩压(SBP)的最大变化。主要终点包括第3个月时死亡或残疾(调整的Rankin量表评分 4-6分)、24小时内神经功能恶化(Glasgow Coma量表评分降低≥2分或美国国立卫生研究院中风量表评分增加≥4分)和7天内急性肾损伤(48小时内血肌酐≥0.3mg/dL或增加≥1.5倍)。
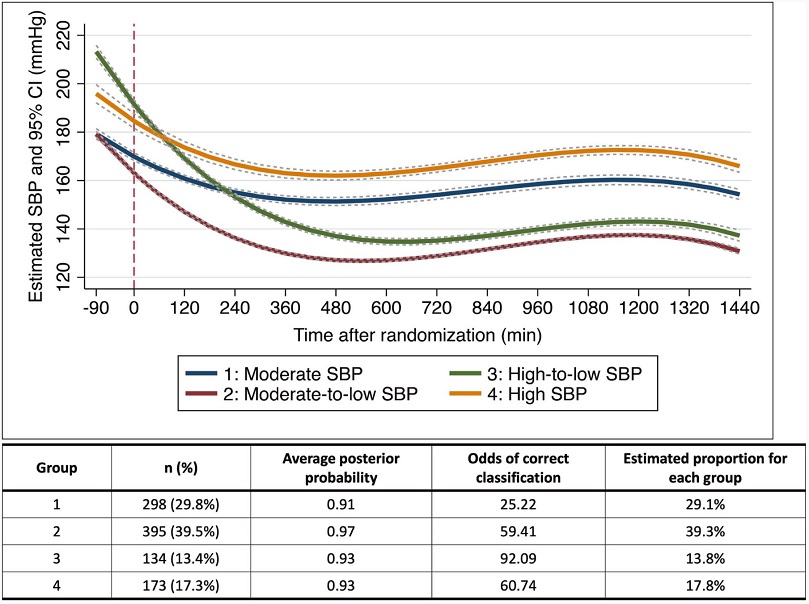
24小时收缩压的变化轨迹
基于组的轨迹建模揭示了4种收缩压变化轨迹:中水平 SBP(从入院到随机分组后:190mmHg→150-160mmHg,n=298)、中→低水平 SBP(190mmHg→<140mmHg, n=395)、高→低水平 SBP(>210mmHg→<140mmHg, n=134)和高水平 SBP(>210mmHg→160-170mmHg,n=173)。
在接受强化降压治疗的患者中,4种收缩压变化轨迹的患者比例分别是11.1%、88.6%、85.1%和1.7%。与中→低水平 SBP组相比,高→低水平 SBP组患者3个月时的死亡或残疾(调整后的OR:2.29)和急性肾损伤(3.50)风险更高,但神经功能恶化风险无明显增加(调整后的OR:0.48)。中水平 SBP和高水平 SBP组的各项预后风险方面均无显著差异。
总之,使用基于组的轨迹建模方法进行数据驱动的观察可能有助于阐明降压治疗、瞬时SBP变化和急性脑出血患者预后之间的相关性。
原始出处:
Kanta Tanaka, et al. Temporal Trajectory of Systolic Blood Pressure and Outcomes in Acute Intracerebral Hemorrhage: ATACH-2 Trial Cohort. Stroke. 2022;53:1854–1862. https://doi.org/10.1161/STROKEAHA.121.037186
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#变化轨迹#
53
#收缩压#
60
#相关性#
43
#患者预后#
56