JAHA:急性心力衰竭患者收缩压与结局的关系
2021-09-13 MedSci原创 MedSci原创
SBP升高与AHF患者良好的短期和长期结局相关。在预先设定的亚组分析中,研究人员发现基线SBP与LVEF≥40%的患者死亡率无关,但与LVEF<40%患者的死亡率密切相关。
在急性心力衰竭(AHF)中,收缩压(SBP)是一个重要的临床变量。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究通过大量AHF患者评估SBP与短期和长期结局之间的关联。
 这项研究是对4项随机对照试验进行的分析,该研究的结局是180天全因死亡率和前14天全因死亡率、心力衰竭恶化或心力衰竭再入院的复合终点。左心室射血分数(LVEF)分为LVEF<40%和LVEF≥40%。多变量Cox回归模型针对AHF结局的已知混杂因素进行了调整。
这项研究是对4项随机对照试验进行的分析,该研究的结局是180天全因死亡率和前14天全因死亡率、心力衰竭恶化或心力衰竭再入院的复合终点。左心室射血分数(LVEF)分为LVEF<40%和LVEF≥40%。多变量Cox回归模型针对AHF结局的已知混杂因素进行了调整。
 该研究共纳入10533名平均年龄为73(±12)岁且平均SBP为145(±7)mmHg的患者。研究人员对9863名患者(93%)进行了LVEF评估;4737名(45%)患者的LVEF<40%。SBP增加与180天死亡率(每增加10mmHg调整后的风险比[HR]为0.93;95%CI为0.89–0.98;P=0.008/10mmHg)和复合终点(每增加10mmHg调整后的HR为0.90;95%CI为0.85–0.94;P<0.001)呈负相关。
该研究共纳入10533名平均年龄为73(±12)岁且平均SBP为145(±7)mmHg的患者。研究人员对9863名患者(93%)进行了LVEF评估;4737名(45%)患者的LVEF<40%。SBP增加与180天死亡率(每增加10mmHg调整后的风险比[HR]为0.93;95%CI为0.89–0.98;P=0.008/10mmHg)和复合终点(每增加10mmHg调整后的HR为0.90;95%CI为0.85–0.94;P<0.001)呈负相关。
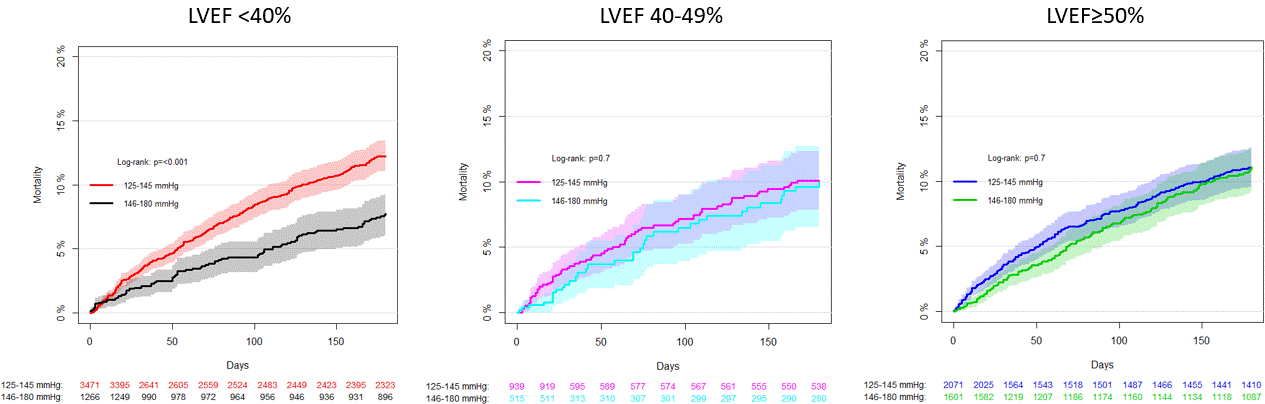 研究人员观察到了SBP与LVEF存在显著的相互作用,表明SBP与LVEF≥40%患者的死亡率无关(每增加10mmHg调整后的HR为0.98;95%CI为0.91-1.04),但与LVEF<40%的患者死亡率增加密切相关(每增加10mmHg调整后的HR为0.84;95%CI为0.77–0.92)。
研究人员观察到了SBP与LVEF存在显著的相互作用,表明SBP与LVEF≥40%患者的死亡率无关(每增加10mmHg调整后的HR为0.98;95%CI为0.91-1.04),但与LVEF<40%的患者死亡率增加密切相关(每增加10mmHg调整后的HR为0.84;95%CI为0.77–0.92)。
由此可见,SBP升高与AHF患者良好的短期和长期结局相关。在预先设定的亚组分析中,研究人员发现基线SBP与LVEF≥40%的患者死亡率无关,但与LVEF<40%患者的死亡率密切相关。
原始出处:
Johannes Grand.et al.Systolic Blood Pressure and Outcome in Patients Admitted With Acute Heart Failure: An Analysis of Individual Patient Data From 4 Randomized Clinical Trials.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.022288
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#收缩压#
48
#AHA#
39
#急性心力衰竭#
50
学习
49
坚持学习
59
坚持学习
57