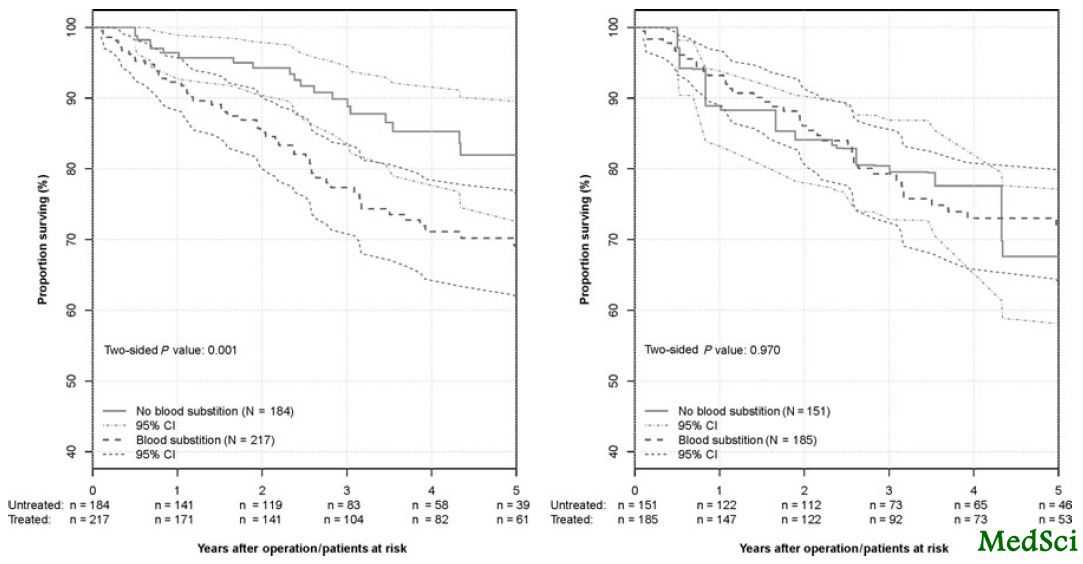
Ann Surg:直肠癌根治性切除术前输血不影响患者生存率
2013-03-21 ecoliDH5 丁香园
患者整体生存率曲线 对于术前输血是否会对患者生存产生不利影响,仍存在较大争议。对此,瑞士圣加伦州立医院的Ignazio Tarantino博士等人通过倾向分数法,评价了术前输血对接受根治性切除术治疗的I-III期直肠癌患者整体生存率及无病生存率的可能影响。该研究结果发表于2013年3月6日在线出版的《外科学年鉴》(Annals of Surgery)杂志上。 该单中心研究对401例I-II

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#切除术#
38
#患者生存#
26
#生存率#
0
#输血#
29
#根治性切除术#
28
#根治#
26